By CAFMI AI From Nature Reviews Endocrinology
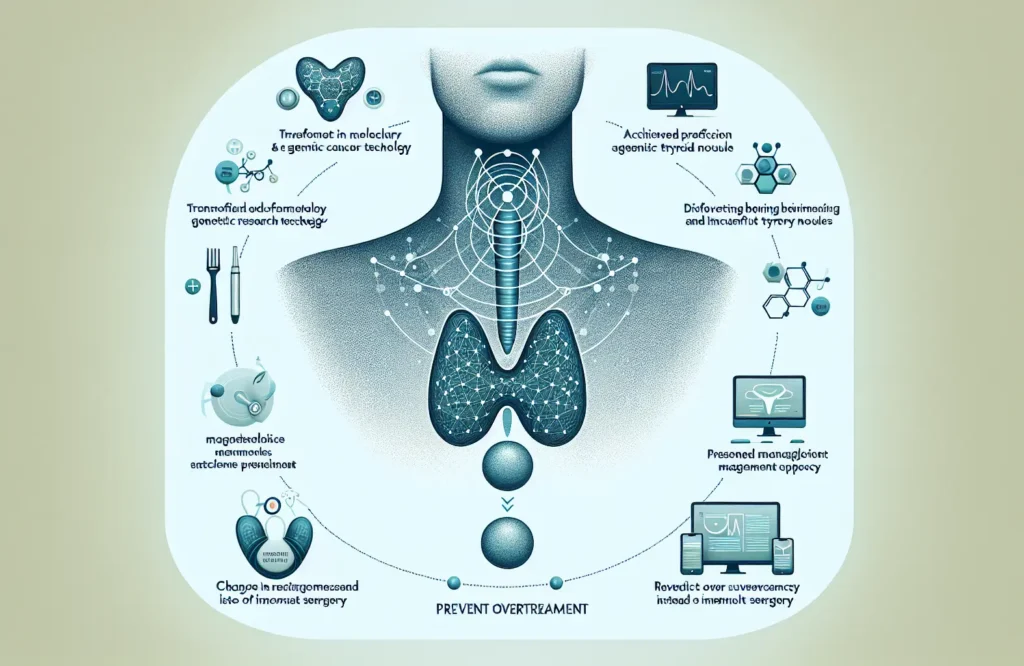
Thyroid cancer management has undergone significant transformation with recent advances in molecular and genetic research. These advances have raised diagnostic accuracy by allowing clinicians to better differentiate between benign and malignant thyroid nodules using molecular testing. Such precision helps prevent overtreatment, especially in cases where nodules might otherwise be surgically removed unnecessarily. The understanding of tumor genetics has also led to refined risk stratification models that categorize thyroid cancers based on their likelihood of progression or recurrence. This stratification is essential for guiding individualized treatment decisions, enabling physicians to tailor interventions according to tumor biology and patient-specific risk factors, rather than relying solely on traditional histopathologic criteria. Active surveillance has gained traction as a management option for low-risk papillary thyroid cancers, reducing the burden of surgery and associated complications for many patients. By monitoring these tumors without immediate surgery, clinicians can balance the need for effective cancer control with the goal of maintaining quality of life. This approach is particularly relevant in the U.S. healthcare context, where overtreatment has been a concern given the increasing incidence of thyroid cancer diagnosis through advanced imaging and biopsy techniques.
Therapeutic advances for thyroid cancer are evolving rapidly, offering new options for patients with advanced or treatment-refractory disease. Several novel targeted therapies, some recently approved and others still under investigation in clinical trials, have shown promise in improving outcomes for patients who do not respond to conventional surgery and radioactive iodine therapy. These targeted agents act on specific pathways involved in tumor growth and spread, representing a shift towards precision oncology in thyroid cancer care. Clinicians, especially in primary and specialty care settings across the U.S., must stay informed about these options to optimize treatment sequencing and management of side effects. Moreover, the integration of multidisciplinary care teams—including endocrinologists, oncologists, surgeons, radiologists, and pathologists—has become pivotal in ensuring comprehensive care. Advanced imaging techniques now complement molecular tests to guide surgical planning, assess treatment response, and facilitate surveillance during follow-up. This coordinated approach helps in balancing treatment efficacy against potential complications and enhances shared decision-making with patients.
The future of thyroid cancer management lies in deeper personalization and integration of emerging technologies. Research is focusing on identifying new biomarkers for even more precise risk assessment and treatment tailoring. Digital health tools, including telemedicine and mobile apps, are enhancing patient engagement and monitoring, particularly for those on active surveillance protocols. Additionally, efforts to improve patient-centered care emphasize addressing quality of life issues, psychosocial support, and clear communication about treatment risks and benefits. Education and training programs continue to evolve to equip healthcare professionals with the knowledge needed to implement these advanced strategies effectively. In the U.S., these trends are shaping a landscape where thyroid cancer care is not only scientifically advanced but also more aligned with the individual patient’s values and preferences.
Read The Original Publication Here