By CAFMI AI From JAMA
Revolutionizing Cystic Fibrosis Treatment with CFTR Modulators
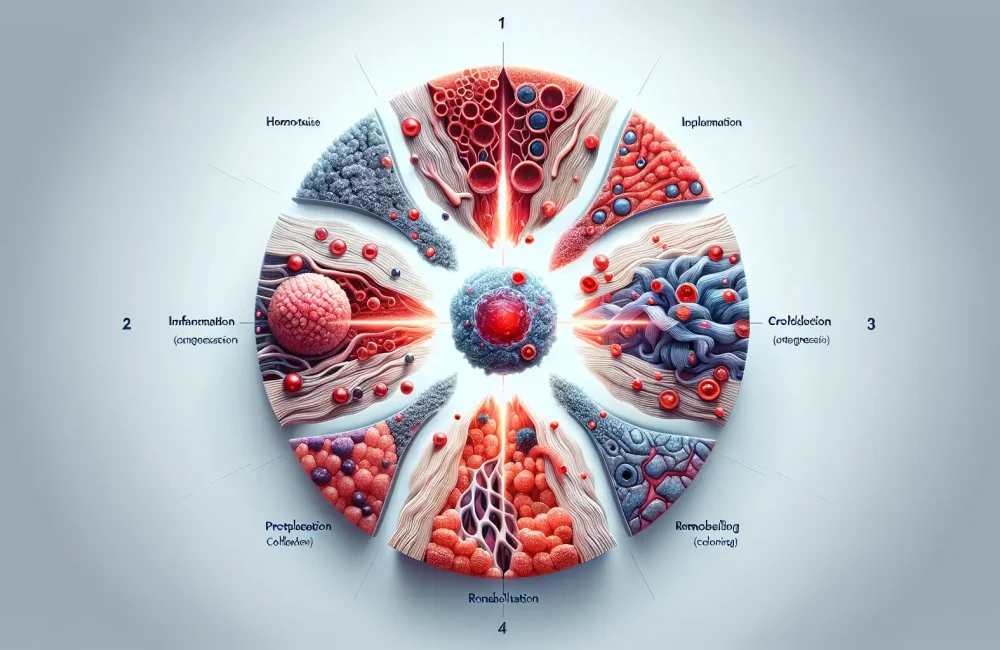
Cystic fibrosis (CF) is a complex genetic disorder caused by mutations in the CFTR gene, leading to significant morbidity predominantly from progressive lung disease and pancreatic insufficiency. Over recent decades, remarkable advances in the understanding of CF pathophysiology have driven transformative changes in therapeutic approaches. Central to these breakthroughs are CFTR modulators, a class of drugs designed to directly correct the underlying defect in the CFTR protein function. These targeted therapies have demonstrated significant benefits for patients by improving lung function, reducing frequency and severity of pulmonary exacerbations, and enhancing overall quality of life. For clinicians in the United States, a key clinical implication is the integration of these modulators into standard care protocols, offering genotype-specific, precision medicine approaches tailored to individual patient mutations. The effective use of CFTR modulators requires careful patient selection, adherence monitoring, and management of potential side effects to optimize outcomes. These agents represent a paradigm shift away from solely symptomatic management toward disease-modifying treatments that address the root cause of CF.
Emerging Gene Therapies and Multidisciplinary Care Advances
Building on the success of CFTR modulators, research has expanded into innovative gene therapy approaches aiming to correct the fundamental genetic defect in CF. This includes vector-mediated gene delivery and novel gene editing techniques currently under evaluation in clinical trials for safety and efficacy. While still in experimental phases, these therapies hold promise for long-term correction and possible cure, rather than lifelong symptomatic treatment. For healthcare providers, awareness of ongoing trials and evolving gene-based treatments is essential to counsel patients accurately, inform referrals to specialist centers, and consider eligibility criteria for participation. Complementing pharmacologic advances are improvements in multidisciplinary care models that bring together pulmonologists, gastroenterologists, nutritionists, physical therapists, and social workers to provide comprehensive individualized management. Early diagnosis through newborn screening has become a critical component ensuring timely intervention, which correlates with better clinical outcomes. Personalized medicine based on genotype and clinical phenotype enables clinicians to tailor therapy, anticipate complications, and implement proactive management strategies effectively.
Challenges and Future Directions in Cystic Fibrosis Management
Despite these advances, significant challenges remain in the management of CF. Persistent chronic infections and inflammatory processes continue to drive lung damage despite current therapies, necessitating ongoing development of novel anti-infective and anti-inflammatory agents. A major clinical concern is ensuring equitable access to cutting-edge treatments such as CFTR modulators and gene therapies across all patient populations, including those underserved or uninsured. Clinicians must stay vigilant for differential diagnoses and red flags during patient evaluation, recognizing comorbid conditions and complications unique to CF. Counseling patients and families about realistic expectations, treatment adherence, and psychosocial support are critical components of effective care. Furthermore, regular follow-up and monitoring protocols must be adapted to incorporate new therapeutic milestones while addressing the evolving needs of patients living longer with CF. The continually rewritten chapter of CF care emphasizes patient-centered approaches, multidisciplinary coordination, and ongoing research collaboration to improve survival and quality of life. For US-based healthcare professionals, understanding these dynamic changes is pivotal to delivering state-of-the-art care and contributing to future innovations targeted at potentially curing this life-shortening disease.
Read The Original Publication Here