By CAFMI AI From New England Journal of Medicine
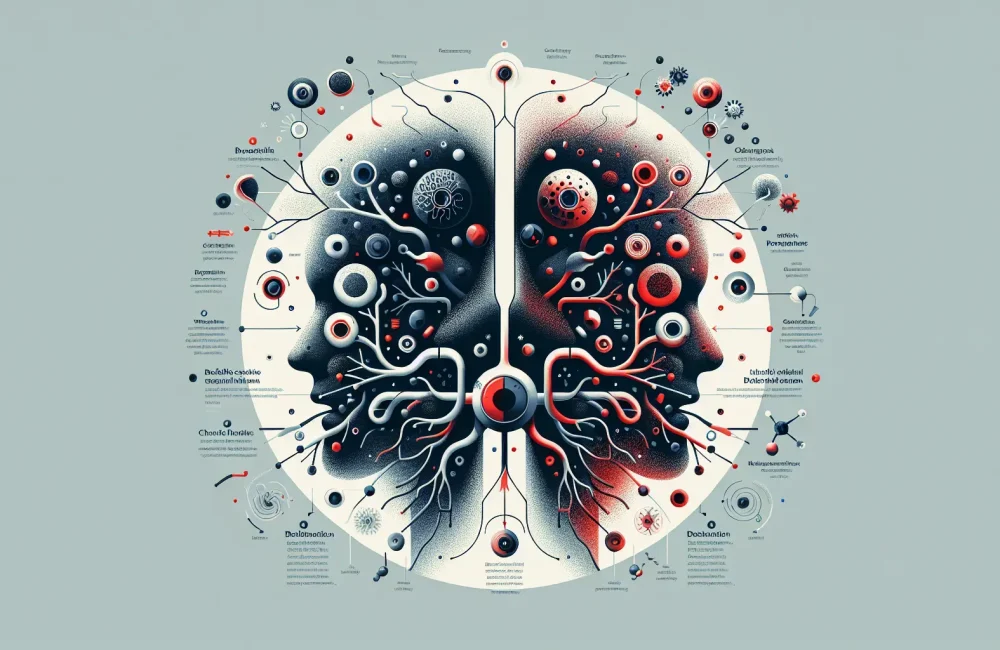
Neutrophilic Inflammation: Central to Bronchiectasis Pathogenesis
Bronchiectasis is a chronic respiratory disorder characterized by permanent bronchial dilation that manifests clinically with symptoms such as persistent cough, sputum production, and recurrent respiratory infections. Central to its pathogenesis is neutrophilic inflammation, which plays a dual role. Neutrophils are vital components of the innate immune defense, protecting the host against invading pathogens. However, their activation and proliferation in bronchiectasis contribute to airway damage and disease progression. When neutrophils become activated, they release various substances including proteases and reactive oxygen species (ROS). These molecules, while aimed at neutralizing pathogens, can cause collateral damage to airway tissues if they are not tightly regulated. This unregulated neutrophilic activity leads to chronic inflammation and structural damage, perpetuating the cycle of infection and injury in the bronchial walls. Understanding this balance between host defense and tissue injury underlines the importance of therapeutic approaches that can moderate neutrophil activity without compromising antimicrobial defense.
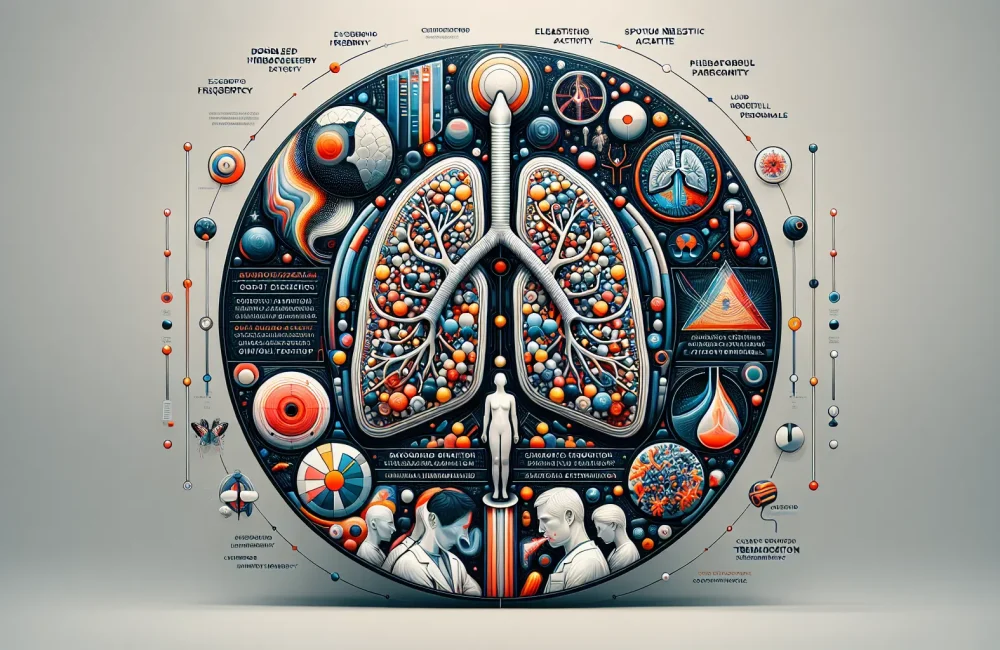
Emerging Therapies: Defanging Neutrophils to Minimize Lung Damage
In recent years, advances in the understanding of neutrophil biology have opened new therapeutic avenues in the management of bronchiectasis. A key target has been neutrophil extracellular traps (NETs), which are web-like structures consisting of DNA, histones, and antimicrobial proteins. While NETs help trap and kill pathogens, they also exacerbate tissue injury and inflammation when overproduced. Therapeutic strategies aim to ‘defang’ neutrophils—preserving their ability to combat infections while reducing the harmful effects on bronchial tissues. Approaches include inhibitors of neutrophil proteases like neutrophil elastase, enzymes critical in degrading airway structures during inflammation. Clinical trials investigating neutrophil elastase inhibitors have demonstrated promising results, including reduction in exacerbation frequency and improvements in lung function, showing potential for modifying disease course. Additionally, agents like recombinant human DNase that degrade NETs have proven beneficial in cystic fibrosis and are currently being evaluated for bronchiectasis. Modulating neutrophil activation through various drugs further complements this strategy, aiming to achieve effective control over airway inflammation and damage.
Future Directions: Balancing Immune Defense and Tissue Protection
Future research in bronchiectasis treatment is focused on achieving a fine balance between maintaining effective immune defense and preventing tissue damage caused by neutrophils. Novel approaches include targeting signaling pathways that regulate neutrophil recruitment and activation, as well as exploring personalized medicine based on patients’ inflammatory profiles. There is growing interest in biomarkers to predict disease progression and response to neutrophil-targeted therapies, enabling more precise and effective treatment plans. Furthermore, combination therapies that address multiple aspects of neutrophil-mediated pathology may provide the best clinical outcomes. Ensuring that treatments do not overly suppress neutrophil function is crucial to avoid increased susceptibility to infections. Overall, integrating these insights holds promise for transforming bronchiectasis management and improving patients’ quality of life.
Read The Original Publication Here