By CAFMI AI From Nature Reviews Disease Primers
Understanding Lung Metastases: Pathophysiology and Diagnosis
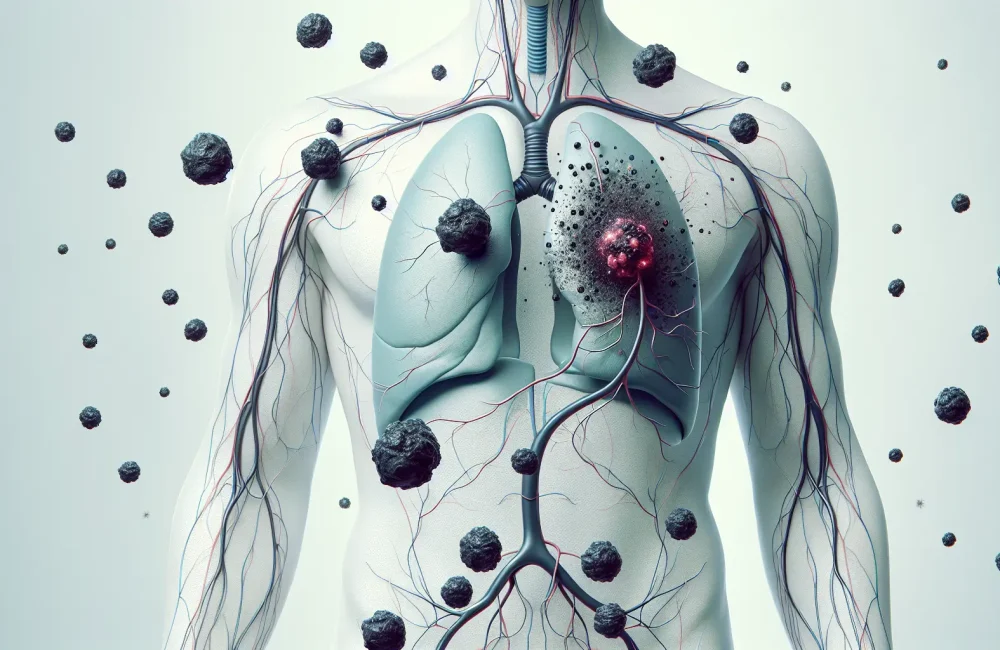
Lung metastases denote secondary cancerous tumors originating from primary malignancies elsewhere in the body, a scenario frequently encountered in clinical oncology. Common primaries include breast cancer, colorectal cancer, and sarcomas. These metastases result from a complex metastatic cascade beginning with detachment of malignant cells from the primary tumor, followed by intravasation into vasculature or lymphatics, survival during systemic circulation, and eventual extravasation into the lung parenchyma where the secondary tumors establish. The lungs provide a distinctive microenvironment facilitating or limiting metastatic colonization through interactions involving tumor cells, stromal elements, and immune defenses. Clinically, patients may be asymptomatic or present with respiratory symptoms, and imaging plays a pivotal role in detection. Modalities such as chest X-rays, computed tomography (CT) scans, and positron emission tomography (PET) scans form the backbone of radiologic assessment. Histopathological confirmation remains essential to differentiate metastatic lesions from primary lung cancers or benign pulmonary nodules. Correct identification of metastatic origin guides appropriate management strategies and prognostic evaluation.
Management Strategies and Therapeutic Considerations
Treatment of lung metastases is multifactorial, primarily influenced by the number, size, and anatomical distribution of pulmonary lesions; the status and resectability of the primary tumor; and the patient’s overall clinical condition including comorbidities and performance status. Surgical resection, often via metastasectomy, is considered potentially curative in selected patients with limited metastatic burden and controlled primary disease. This approach requires careful patient selection and multidisciplinary evaluation. Systemic therapies including traditional chemotherapy regimens remain a cornerstone for controlling widespread metastatic disease and alleviating symptoms. Additionally, advances in targeted therapies and immunotherapy are altering treatment paradigms by offering personalized options based on tumor molecular profiles. Radiation therapy serves as an adjunct or palliative option in certain scenarios. Integrating these modalities demands nuanced clinical judgment to optimize outcomes and balance treatment-related morbidities.
Prognosis and Future Directions in Lung Metastases Research
The prognosis of patients with lung metastases depends largely on factors such as primary tumor type, metastatic burden, response to therapy, and patient performance status. While some patients achieve long-term survival following aggressive local and systemic treatments, others experience rapid disease progression. Ongoing research focuses on uncovering the molecular mechanisms underlying metastatic spread and resistance, aiming to identify novel biomarkers for early detection and therapeutic targets. Emerging approaches include the utilization of liquid biopsies for monitoring tumor dynamics, development of next-generation targeted agents, and enhancing immunotherapeutic strategies. Multidisciplinary collaboration remains essential to translate these scientific advances into clinical practice, ultimately improving survival and quality of life for patients affected by lung metastases.
Read The Original Publication Here