By CAFMI AI From JAMA
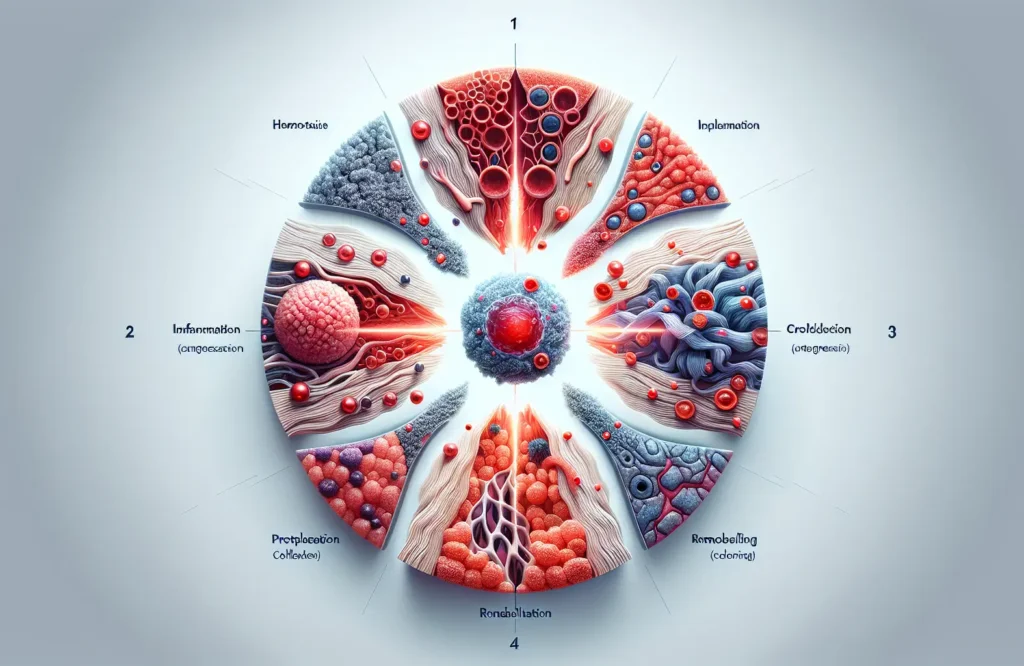
Wound healing is a complex physiological process essential for tissue repair and recovery following injury. Clinicians should be aware that healing occurs in four main phases: hemostasis, inflammation, proliferation, and remodeling. Hemostasis begins immediately after injury to stop bleeding through vasoconstriction and clot formation. The inflammatory phase follows, where immune cells clear debris and pathogens, crucial for preventing infection but potentially detrimental if prolonged. Next, the proliferative phase involves tissue regeneration, angiogenesis, and formation of granulation tissue, laying the foundation for new tissue. Finally, remodeling strengthens the tissue over time, realigning collagen fibers to restore skin integrity. Understanding these phases helps clinicians identify atypical healing patterns, such as delayed inflammation or impaired proliferation, which may indicate complications or underlying conditions like diabetes, malnutrition, or vascular insufficiency. Recognizing such deviations early enables timely intervention to prevent chronic wound formation.
Recent advancements in wound care have introduced novel therapies that significantly improve outcomes for both acute and chronic wounds. These include bioengineered skin substitutes, which serve as scaffolds to promote cell growth and accelerate healing, particularly useful in extensive or non-healing wounds. Advanced dressings, such as hydrocolloids, foam dressings, and antimicrobial-impregnated materials, provide occlusion, moisture balance, and infection control tailored to wound characteristics. Negative pressure wound therapy (NPWT) has revolutionized complex wound treatment by enhancing circulation, reducing edema, and stimulating granulation tissue through controlled suction. Clinicians should integrate these modalities based on wound etiology, size, and patient factors to maximize effectiveness. The article also highlights the importance of managing infection risk and systemic factors like diabetes control and nutrition, which significantly impact healing trajectories. Case studies illustrate how combining these approaches with thorough assessment and monitoring can optimize results and reduce complications.
For healthcare professionals, staying informed about evolving wound care practices is critical to improving patient quality of life and resource utilization. This article emphasizes the need for personalized treatment protocols that consider patient-specific variables such as comorbidities, lifestyle, and wound characteristics. Challenges remain in standardizing care due to variability in wound types and healing responses, underscoring the importance of continuing education and research. Clinicians should also remain vigilant for red flags such as signs of infection, poor perfusion, and non-healing ulcers, prompting referral or advanced therapies. Follow-up care involves regular reassessment and adjustment of treatment plans to address evolving wound needs. The article advocates for increased clinical trials to validate emerging technologies and the development of integrated primary care workflows for chronic wound management. Counseling patients on wound care, risk factor modification, and adherence enhances outcomes. As wound care advances, multidisciplinary collaboration will be pivotal in translating innovations into routine practice to ultimately reduce morbidity and healthcare costs.
Read The Original Publication Here