By CAFMI AI From JAMA
Significant Reduction in Lipoprotein(a) Levels
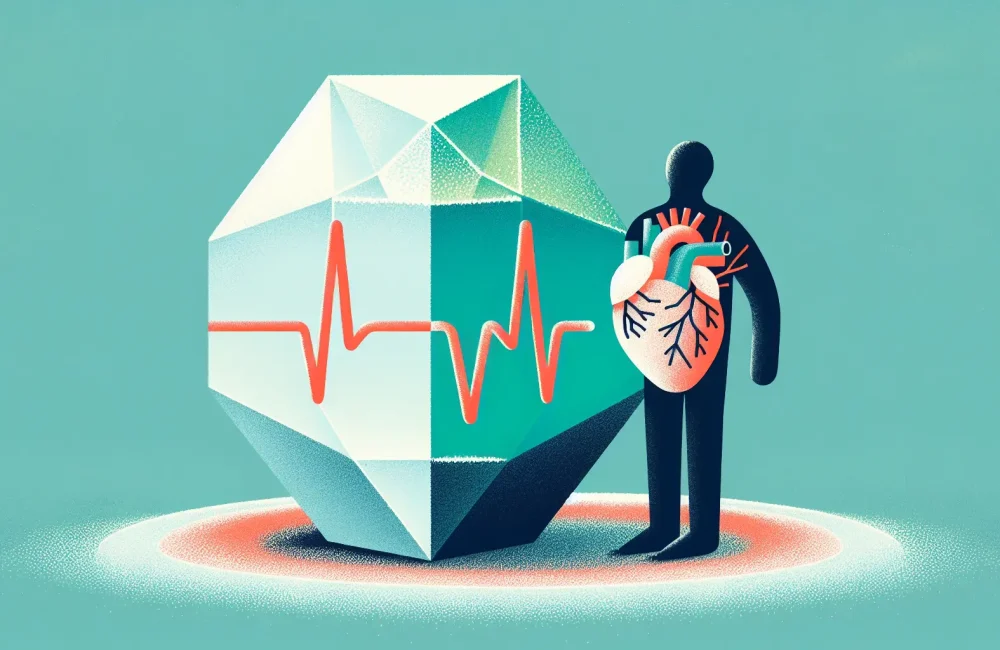
Elevated Lipoprotein(a) [Lp(a)] is a recognized independent risk factor for atherosclerotic cardiovascular disease, contributing to increased morbidity and mortality worldwide. Despite the established link between high Lp(a) concentrations and cardiovascular risk, therapeutic options targeting Lp(a) have been limited, leaving a substantial gap in preventive cardiology. The recent randomized clinical trial investigating oral Muvalaplin offers promising insights into effective management strategies for patients with elevated Lp(a). The trial focused on adults with elevated baseline Lp(a) levels, administering Muvalaplin over a 12-week treatment period and comparing outcomes with a placebo group. Results revealed a significant and statistically robust reduction in Lp(a) levels among patients receiving Muvalaplin compared to placebo, marking a breakthrough in the effort to specifically lower this lipid marker. This reduction is clinically meaningful, given the direct association between Lp(a) concentrations and cardiovascular events such as myocardial infarction and stroke. These findings may redefine risk stratification and therapeutic approaches in cardiovascular medicine, particularly for populations who continue to experience cardiovascular events despite standard lipid-lowering therapies. The trial also verified the safety and tolerability of Muvalaplin, which is essential for its potential integration into clinical practice. The side effect profile was acceptable, with no unexpected adverse events, underscoring the potential of Muvalaplin as a viable oral therapeutic option.
Broader Cardiovascular Benefits and Mechanistic Insights
Beyond Lp(a) reduction, the trial assessed secondary outcomes including changes in low-density lipoprotein cholesterol (LDL-C) and inflammatory markers, both critical components in cardiovascular risk. The data indicated favorable shifts in LDL-C levels and a decrease in inflammatory biomarkers in the Muvalaplin group, supporting the notion that lowering Lp(a) could confer broader cardioprotective effects. Inflammatory processes play a pivotal role in atherogenesis and plaque instability, and thus, therapies that modify inflammation alongside lipid profiles hold enhanced promise for reducing cardiovascular events. These results emphasize the multifaceted impact of Muvalaplin, suggesting benefits that extend beyond simple Lp(a) lowering to favorably altering key pathophysiological mechanisms underlying cardiovascular disease. The authors detailed the mechanism of action of Muvalaplin, which involves modulation of lipid metabolism pathways leading to reduced Lp(a) production or enhanced clearance. Additionally, the pharmacokinetics of oral Muvalaplin demonstrate consistent absorption and bioavailability, enabling convenient dosing regimens conducive to patient adherence. Understanding these mechanistic underpinnings not only clarifies how Muvalaplin achieves its effects but also assists clinicians in identifying suitable candidates for therapy and anticipating clinical outcomes.
Implications for Clinical Practice and Future Research
The trial’s positive outcomes position Muvalaplin as a potential cornerstone in managing patients with elevated Lp(a), a group historically underserved by existing lipid-lowering therapies. Incorporation of Muvalaplin into clinical practice could improve cardiovascular risk profiles and reduce event rates in this high-risk population. However, longer-term studies and real-world evidence are necessary to confirm sustained efficacy, safety, and impacts on hard clinical endpoints such as myocardial infarction, stroke, and cardiovascular mortality. Future research directions include exploring combination therapies with existing lipid-lowering agents, investigating Muvalaplin’s effects in diverse populations with varying cardiovascular risk factors, and elucidating further the molecular mechanisms governing Lp(a) metabolism. The advancement represented by Muvalaplin exemplifies the ongoing evolution in precision cardiovascular medicine, aiming for targeted therapies that address specific pathogenic pathways, ultimately enhancing patient outcomes and reducing the global burden of cardiovascular disease.
Read The Original Publication Here