By CAFMI AI From Gut
Novel Risk Stratification for HCC in MASLD Patients
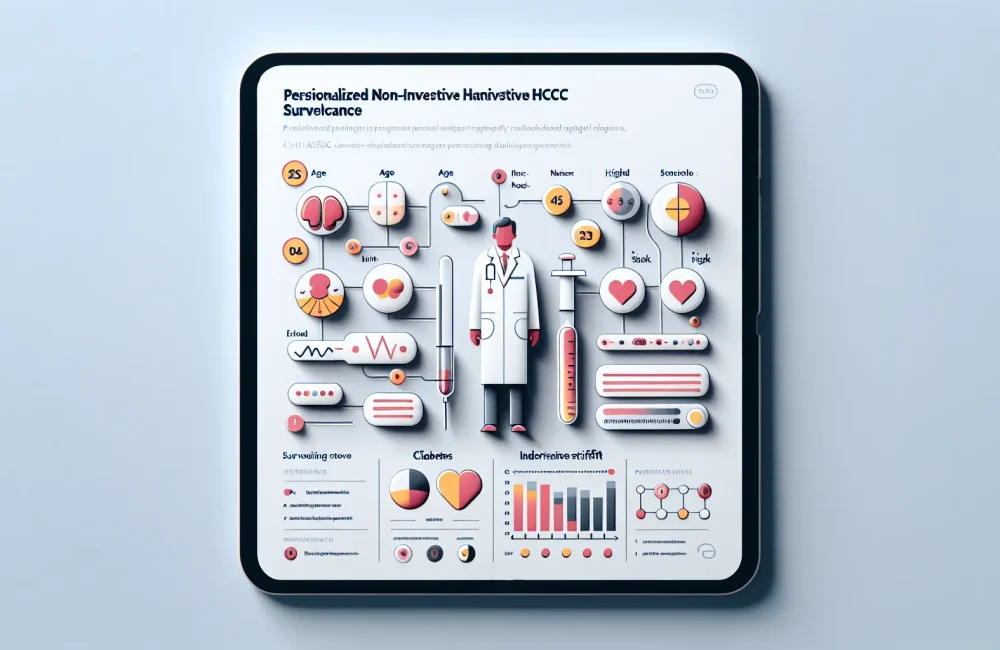
Metabolic dysfunction-associated steatotic liver disease (MASLD) is rapidly emerging as a predominant contributor to hepatocellular carcinoma (HCC) incidence, surpassing traditional causes such as viral hepatitis in many regions, including the United States. This shift warrants a critical reassessment of HCC surveillance strategies, which have historically been modeled after viral liver disease paradigms and may thus inadequately address the distinct risk profile of MASLD patients. Recognizing this gap, the study at hand undertook a robust multicenter prospective cohort investigation involving 3,200 MASLD patients monitored over a median period of five years. The primary goal was to develop and validate a non-invasive, risk-based surveillance tool specifically tailored to this growing patient population. A comprehensive set of variables encompassing clinical, biochemical, and imaging data were prospectively collected and analyzed. Significant factors independently predicting HCC development included advanced age, the presence of diabetes mellitus—a common comorbidity in MASLD—elevated serum alpha-fetoprotein (AFP), liver stiffness measurements via elastography, and platelet counts. Employing multivariable Cox regression and rigorous internal validation through bootstrap resampling ensured the derived risk model was both statistically robust and clinically relevant. The resulting stratification classified patients into low-, intermediate-, and high-risk groups for HCC incidence, demonstrating significant incidence rate disparities (p<0.001). Importantly, the model exhibited excellent discriminative capability, reflected by a c-statistic of 0.82, and accurate calibration, confirming the reliability of risk predictions across different patient strata.
Clinical Impact and Implementation of Risk-Based Surveillance
For clinicians, especially those practicing in the United States where MASLD prevalence is rising, the findings from this study offer a transformative approach to HCC surveillance. The risk model’s non-invasive nature—leveraging serum biomarkers, elastography, and routine clinical parameters—facilitates its practical integration into primary and specialty care workflows without imposing additional procedural burdens on patients. The delineation of patients into risk tiers enables clinicians to personalize surveillance intensity, focusing resources and imaging modalities such as ultrasound and cross-sectional imaging on individuals most likely to develop HCC, while potentially reducing unnecessary surveillance in low-risk groups. This personalized surveillance paradigm promises to enhance early tumor detection rates, thereby improving therapeutic options and patient outcomes. Decision curve analysis supported the clinical utility of applying this model, providing quantifiable net benefits over existing one-size-fits-all approaches. Furthermore, recognizing the interplay between metabolic comorbidities and liver cancer risk empowers multidisciplinary care coordination involving endocrinologists, hepatologists, and primary care providers, facilitating comprehensive management of MASLD patients beyond surveillance alone.
Future Directions and Broader Implications
Looking ahead, further validation of the risk-based surveillance model in diverse populations and healthcare settings is needed to confirm its generalizability and cost-effectiveness. Integrating emerging biomarkers, genetic profiling, and advanced imaging techniques may further refine risk prediction and early HCC detection. Additionally, this approach underscores the necessity of addressing metabolic health comprehensively, as lifestyle interventions and pharmacologic therapies targeting MASLD and its metabolic comorbidities could modify HCC risk trajectories. Policymakers and healthcare systems should consider adopting risk-based surveillance guidelines to optimize resource allocation and improve outcomes for MASLD patients. Ultimately, this paradigm shift from uniform to individualized surveillance could serve as a model for other cancer screening programs affected by changing epidemiology and patient heterogeneity.
Read The Original Publication Here