By CAFMI AI From Frontiers in Medicine (Open Access)
Comprehensive Health Metrics and Kidney Stone Risk
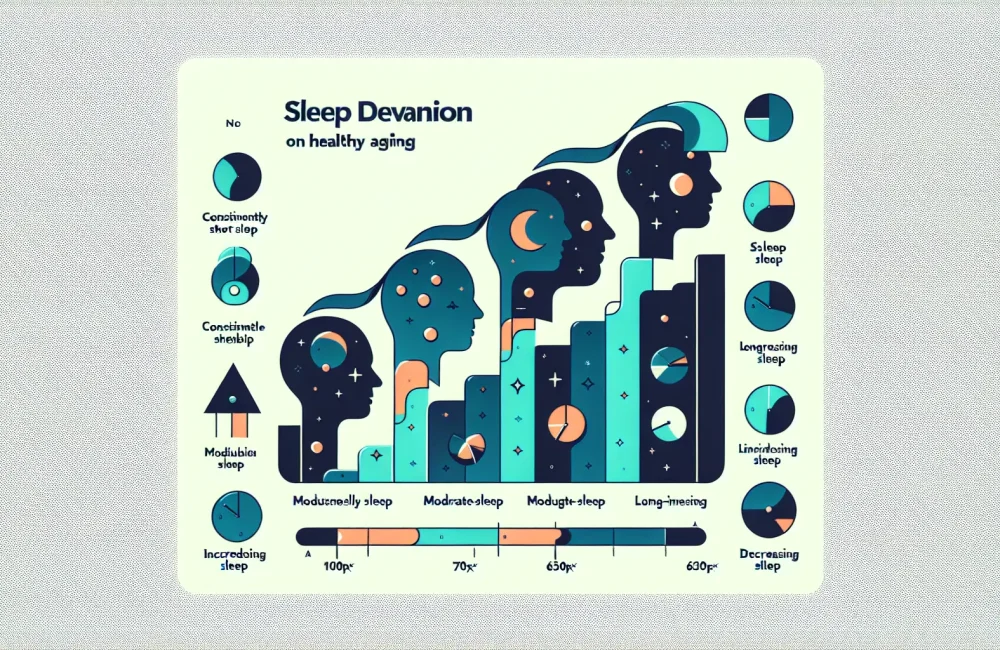
Kidney stones are a prevalent urological condition causing considerable pain and potential complications such as urinary tract infections and kidney damage. This population-based study investigated the association between the Life’s Crucial 9 (LC9) health metrics—a set of nine essential cardiovascular health factors defined by the American Heart Association—and the prevalence of kidney stones. The LC9 metrics include smoking status, body mass index (BMI), physical activity, diet, total cholesterol levels, blood pressure, blood glucose, sleep quality, and mental health. The study employed a cross-sectional design using data derived from a large, representative health survey. Participants were assessed on their adherence to each LC9 metric and grouped accordingly. Kidney stone presence was determined by self-report, which was corroborated with medical imaging records when available, ensuring more reliable outcome classification.
The study’s findings show a clear inverse relationship between adherence to the LC9 metrics and kidney stone prevalence. Individuals who achieved higher conformity to the ideal standards of LC9 exhibited significantly lower rates of kidney stones compared to those with poor adherence. Notably, non-smoking status, maintaining a healthy body weight, engaging in adequate physical activity, and controlling blood pressure demonstrated the strongest protective associations against kidney stones. These results underscore the importance of a lifestyle that simultaneously targets multiple health factors rather than isolated interventions. For clinicians, these findings emphasize the utility of a composite health metric approach in assessing kidney stone risk during routine evaluations, particularly for patients with recurrent stones or other risk factors.
Clinical Implications and Preventive Strategies
From a clinical perspective, the association between the Life’s Crucial 9 metrics and kidney stone risk introduces practical opportunities for preventive care. Given that these metrics encompass modifiable lifestyle and physiological factors, healthcare providers—especially those in primary care and urology—can implement targeted counseling and interventions aimed at comprehensive health improvement. For example, smoking cessation programs, weight management through tailored physical activity regimes, nutritional guidance promoting kidney stone-friendly diets, and vigilant blood pressure and glucose monitoring are all actionable elements within the LC9 framework. The interplay of these factors suggests that integrated management plans may be more effective in reducing kidney stone incidence than addressing single risk factors in isolation.
Moreover, this study encourages clinicians to incorporate assessment of these nine components into routine patient evaluations, particularly for populations at elevated risk for nephrolithiasis. Screening for mental health and sleep quality, components often overlooked in kidney stone risk evaluation, may offer additional avenues for holistic patient care. The evidence supports multidisciplinary approaches involving dietitians, physiotherapists, and behavioral health specialists to optimize patient adherence to LC9 guidelines. Clinicians should be mindful of the study’s limitations, such as its cross-sectional nature that precludes causal inferences and reliance on self-reported stone history in some cases. Nonetheless, the strong associations found provide a robust rationale for emphasizing LC9 adherence in preventive strategies.
Broader Context and Future Directions in Patient Care
Kidney stone formation is influenced by complex interactions between genetic, environmental, and lifestyle factors. The Life’s Crucial 9 metrics present a novel, multifactorial approach to understanding and mitigating kidney stone risk. The study highlights that achieving ideal cardiovascular health markers can have substantial benefits beyond heart disease prevention, extending to urological health. This holistic health model aligns with the growing emphasis on integrative care that addresses multiple comorbidities and patient-centered outcomes.
Future research should focus on longitudinal studies to establish causal links and evaluate the impact of interventions targeting the LC9 metrics specifically on kidney stone incidence and recurrence rates. Additionally, incorporating LC9 assessments into clinical guidelines for kidney stone management could standardize the role of lifestyle and metabolic health in reducing disease burden. Primary care workflows should consider embedding brief LC9 screening tools to facilitate early identification of at-risk patients and the prompt initiation of multifaceted prevention programs. Patient counseling should be enhanced with education on the importance of combined lifestyle factors—such as diet quality, physical activity, and sleep hygiene—in kidney stone prevention. This comprehensive approach may ultimately reduce healthcare costs and improve patient quality of life by addressing kidney stones as part of overall cardiovascular and metabolic health maintenance.
Read The Original Publication Here