By CAFMI AI From Nature Reviews Nephrology
Revolutionizing Diagnosis Through Antigen Discovery
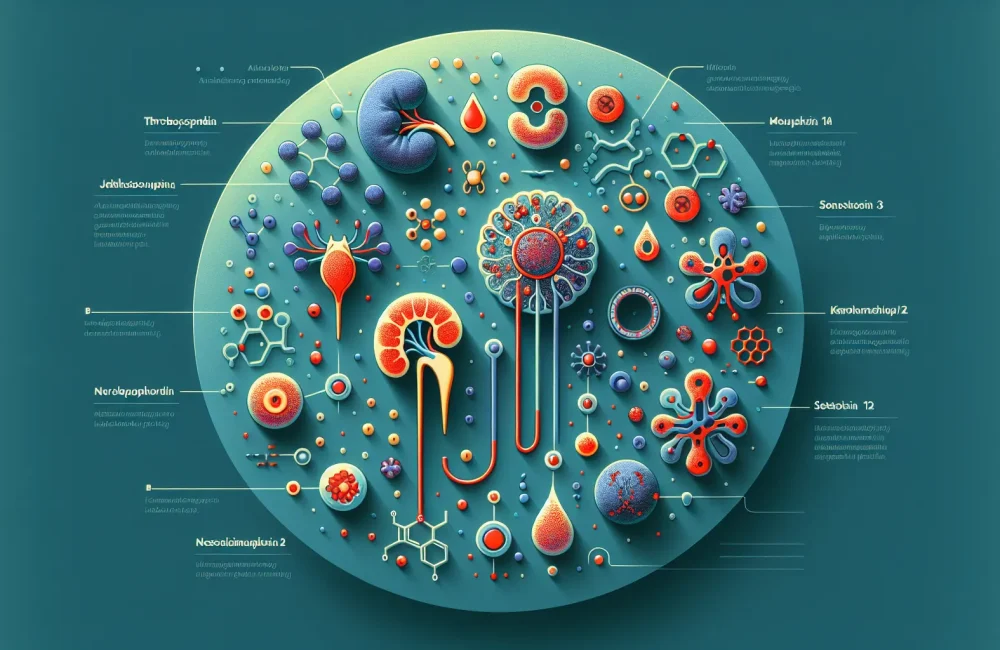
Membranous nephropathy (MN) is a primary cause of nephrotic syndrome in adults, defined by the presence of subepithelial immune deposits on the glomerular basement membrane. Recent advances have dramatically evolved the understanding and management of MN, largely due to the identification of specific target antigens. Initially, the discovery of the M-type phospholipase A2 receptor (PLA2R) marked a milestone, establishing it as a major antigen in idiopathic MN and a critical diagnostic and therapeutic marker. Following this, further research expanded the landscape of MN antigens to include thrombospondin type-1 domain-containing 7A (THSD7A), neural epidermal growth factor-like 1 protein (NELL-1), semaphorin 3B, and exostosin 1/exostosin 2 (EXT1/EXT2) among others. Each antigen presents unique pathological features and clinical implications that aid in disease classification and prognosis.
The discovery of these antigens involved sophisticated techniques such as mass spectrometry-based proteomics, laser-capture microdissection of glomeruli, and immunological validation methods. The identification of antigen-specific antibodies has crucial clinical applications — these antibodies not only assist in confirming a diagnosis of MN but also help in predicting disease activity and monitoring response to therapy. Moreover, antigen profiles are often linked to distinct clinical phenotypes and associated systemic diseases, underlining the importance of a tailored diagnostic approach. This antigen-driven classification refines previous idiopathic categorizations, offering a more precise framework to guide patient care.
Clinical Applications and Diagnostic Strategy
From a clinical perspective, antibody testing against PLA2R and THSD7A is now established in the standard diagnostic workflow for membranous nephropathy. These serological tests serve to confirm MN diagnosis, anticipate disease severity, and evaluate therapeutic effectiveness. In cases where patients are negative for PLA2R antibodies, newer antigens have been identified, helping to clarify the etiology in these previously idiopathic cases. The ongoing discovery of antigens enriches the diagnostic repertoire, enabling more personalized assessments and prognosis predictions.
The impact on clinical workflow is significant; utilizing serological markers allows clinicians to monitor disease progression more closely and intervene timely with immunosuppressive therapies tailored to the patient’s antigen profile and antibody titers. This approach contrasts traditional treatment that often relied heavily on histological findings alone. The stratification based on antigen presence also influences prognostic outlooks, where certain antigen profiles correlate with disease course and likelihood of remission or relapse. This nuanced understanding equips healthcare professionals with a deeper insight into patient-specific disease mechanisms and treatment needs.
Therapeutic Implications and Future Directions
Therapeutically, the identification of target antigens in MN fosters an era of precision medicine, where immunosuppressive regimens are increasingly tailored to the individual’s antigen status and serologic response. Monitoring circulating antibody levels offers an opportunity for earlier detection of relapse or remission, enabling clinicians to adjust treatment proactively rather than reactively. This paradigm supports better patient outcomes and minimizes unnecessary drug exposure.
Further, advances in understanding antigen-specific immune pathways are opening innovative avenues for therapy beyond conventional immunosuppression. These include strategies focused on inducing immune tolerance or selective B cell depletion targeting the responsible antibodies, which could reduce side effects and improve long-term treatment efficacy. Importantly, ongoing research continues to uncover new antigens, promising to further stratify MN subtypes and refine therapeutic strategies. This evolution may soon translate into more effective and personalized management protocols, thereby enhancing quality of life and prognosis for patients with membranous nephropathy.
Read The Original Publication Here