By CAFMI AI From JAMA
Frailty and Its Link to Dementia Risk
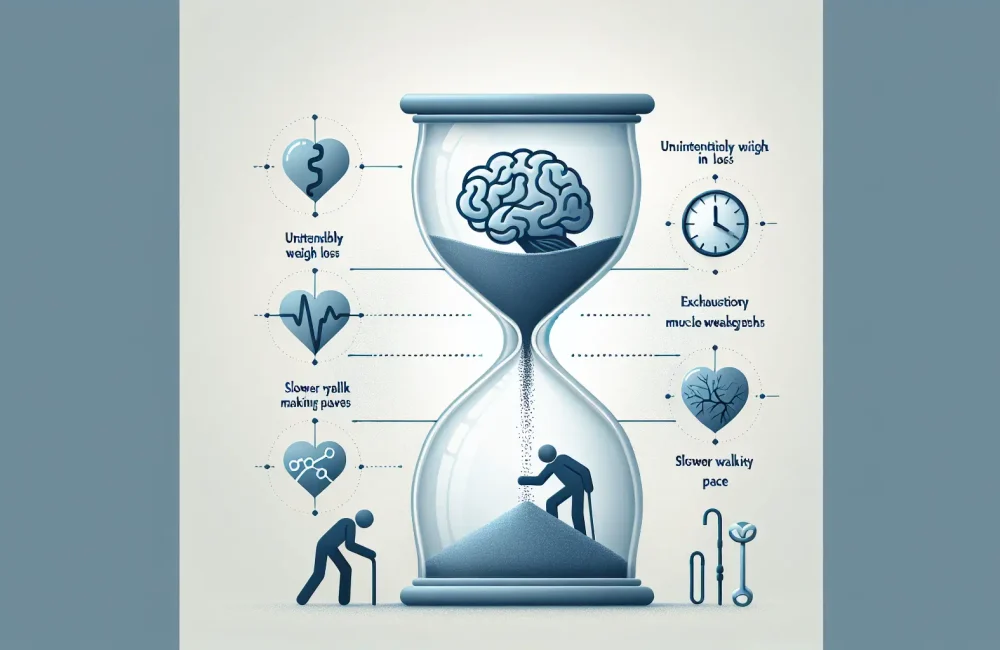
Frailty is a common clinical syndrome in older adults characterized by decreased physiological reserve and increased vulnerability to adverse health outcomes, including disability, hospitalization, and death. This study focused on examining the relationship between key frailty symptoms and the risk of developing dementia over time. The frailty symptoms evaluated included unintentional weight loss, exhaustion, muscle weakness, slowness in walking, and low levels of physical activity. Researchers followed a cohort of elderly participants for several years, assessing these physical indicators and monitoring the incidence of dementia diagnoses. Their findings revealed a strong association between the presence of frailty symptoms and heightened risk for cognitive decline and dementia. Individuals exhibiting one or more frailty symptoms were significantly more likely to experience dementia onset compared to those without these symptoms. This relationship persisted even after adjusting for other potential confounding factors such as age, sex, and comorbidities. The study underlines that frailty represents more than physical vulnerability — it is a potential marker for future neurodegenerative disease risk. The recognition of frailty symptoms during clinical evaluations can therefore act as an early warning sign, prompting further cognitive assessment and closer follow-up for at-risk patients.
Clinical Implications and Management Strategies
The association found between frailty symptoms and elevated dementia risk carries important implications for clinical practice, especially in primary care and geriatrics settings. Early identification of frailty symptoms offers clinicians an opportunity to intervene before significant cognitive decline occurs. Routine frailty assessments should be incorporated as part of comprehensive geriatric evaluations, using simple tools that evaluate weight changes, fatigue, grip strength, gait speed, and physical activity levels. From a management standpoint, addressing frailty could potentially reduce or delay the progression to dementia. Interventions targeting physical health, such as tailored exercise programs to improve muscle strength and endurance, nutritional optimization to address weight loss and deficiencies, and strategies to reduce exhaustion, are recommended. Additionally, clinicians should consider multidisciplinary approaches involving physical therapists, dietitians, and social support services to create holistic care plans that address both physical and cognitive health components. Educating patients and caregivers about the connection between frailty and dementia risk empowers them to engage in preventative strategies and maintain functional independence longer. Moreover, awareness of this link enhances monitoring for early signs of cognitive impairment during routine visits, facilitating timely diagnosis and appropriate management.
Research Context, Limitations, and Future Directions
This study contributes to the growing body of evidence supporting the interconnectedness of physical frailty and cognitive decline. It highlights the need for a holistic approach in aging research and clinical care by integrating assessments of physical and cognitive health. However, certain limitations should be considered when interpreting the results. The observational design means causality cannot be definitively established; frailty symptoms may coexist with early, undetected neurodegeneration rather than directly causing dementia. The cohort studied was limited to elderly individuals, and findings may not generalize to younger populations or those with different demographic characteristics. Future research should aim to elucidate the biological mechanisms linking frailty and dementia, potentially exploring inflammatory pathways, vascular contributions, and neurodegenerative processes. Trials evaluating the effectiveness of frailty-targeted interventions for dementia prevention are needed to clarify whether improving physical health can alter cognitive outcomes. In clinical practice, these findings support guidelines endorsing proactive frailty screening and integrated care pathways to manage older adults comprehensively. Counseling patients about red flags such as sudden worsening of physical function or cognitive complaints is essential, as is planning regular follow-up appointments to assess both frailty progression and cognitive status. This integrated approach could improve quality of life and reduce healthcare burden associated with dementia and frailty in aging populations.
Read The Original Publication Here