By CAFMI AI From npj Parkinson’s Disease (Open Access)
Advanced Imaging Techniques Identify Early PD Markers
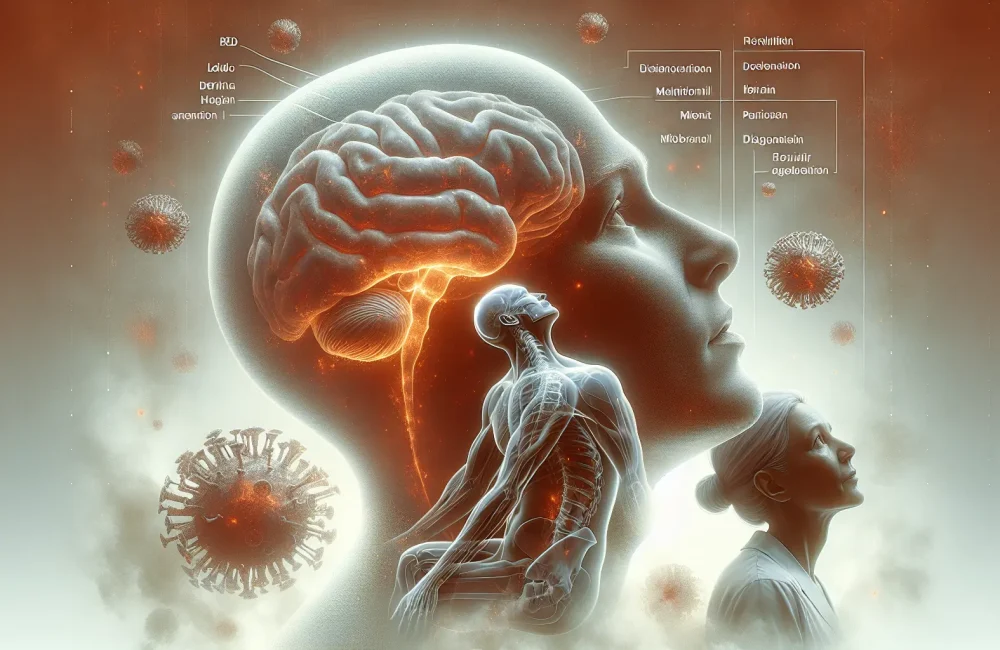
Parkinson’s disease (PD) is widely known for its motor symptoms such as tremors and rigidity, but recent research highlights that non-motor symptoms can manifest years before these classic signs appear. This prodromal phase, involving symptoms like REM sleep behavior disorder, hyposmia (loss of smell), constipation, and mood changes, offers a critical window for early diagnosis and intervention to potentially alter disease progression. Recent advances in imaging technology have provided powerful tools to detect these early non-motor markers with greater accuracy and specificity than ever before. Modalities including positron emission tomography (PET), single-photon emission computed tomography (SPECT) with dopamine transporter ligands, and advanced magnetic resonance imaging (MRI) sequences are at the forefront of this progress. These imaging techniques allow clinicians and researchers to visualize subtle changes in brain regions implicated early in PD — such as the olfactory bulb, autonomic nervous system structures, and brainstem nuclei — which are otherwise difficult to assess clinically. Detecting such changes with modern imaging can help confirm prodromal PD diagnosis in patients presenting with non-specific symptoms, thus facilitating earlier and more targeted clinical management strategies. For U.S.-based clinicians, awareness of these modalities presents an opportunity to refine diagnostic workflows for patients presenting with prodromal or ambiguous symptoms suggestive of Parkinson’s disease.
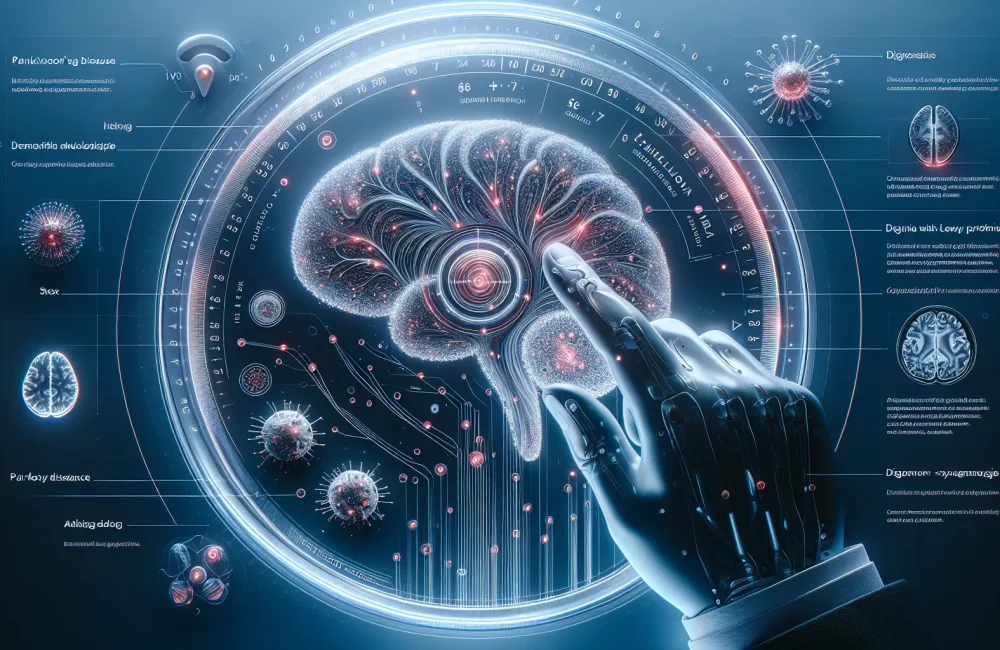
Clinical Implications and Integration of Multimodal Biomarkers
The integration of advanced imaging with clinical assessments and biochemical biomarkers significantly boosts the sensitivity and specificity of early PD diagnosis. Beyond visualizing structural and functional brain changes, combining imaging data with biomarkers like alpha-synuclein levels and autonomic function testing helps clinicians create a comprehensive picture of prodromal PD. This multimodal approach reduces diagnostic uncertainty and opens avenues for stratifying patients according to progression risk, enabling personalized monitoring and therapeutic planning. Clinically, these imaging advances enable earlier identification of patients who might benefit from neuroprotective therapies before substantial neuronal loss occurs. Therapeutic translation based on imaging biomarkers is an exciting frontier, focusing on interventions designed to modify disease trajectory during the prodromal phase. Currently, disease-modifying treatments for PD remain limited; however, identifying prodromal markers through imaging helps design clinical trials targeting early-stage interventions. This proactive strategy emphasizes preventing or slowing disease progression rather than managing symptoms after motor onset. For frontline clinicians, leveraging evidence-informed imaging biomarkers facilitates patient counseling on prognosis and therapy expectations, while also guiding referrals to specialized care or research studies. Furthermore, understanding the spectrum and timing of non-motor symptoms captured by imaging can aid differential diagnosis, ruling out other neurodegenerative disorders that may mimic PD symptoms early on.
Challenges, Future Directions, and Impact on Primary Care
Despite the promise of imaging advances in prodromal PD detection, several challenges remain before widespread clinical adoption. Variability in imaging protocols and lack of standardized criteria across institutions can hinder reproducibility and comparability of findings. Longitudinal studies are essential to validate imaging markers’ predictive value and understand how changes correlate with disease progression and response to therapies. Collaborative multicenter efforts and the use of machine learning for sophisticated image analysis hold great potential to overcome these limitations, enhancing diagnostic accuracy and enabling large-scale application. Moreover, incorporating these imaging tools into primary care workflows demands practical guidelines and training for clinicians, especially in community settings where access to advanced neuroimaging may be limited. Counseling patients on the implications of prodromal PD findings requires nuanced communication to balance early detection benefits against anxiety related to a neurodegenerative diagnosis without guaranteed progression. Ultimately, these imaging advances could revolutionize care paradigms by shifting focus toward prevention and early intervention, improving quality of life through timely therapeutic strategies. For U.S.-based healthcare providers, staying informed on these evolving modalities will be critical to optimizing patient outcomes in Parkinson’s disease management as new evidence and technologies emerge.
Read The Original Publication Here