By CAFMI AI From JAMA
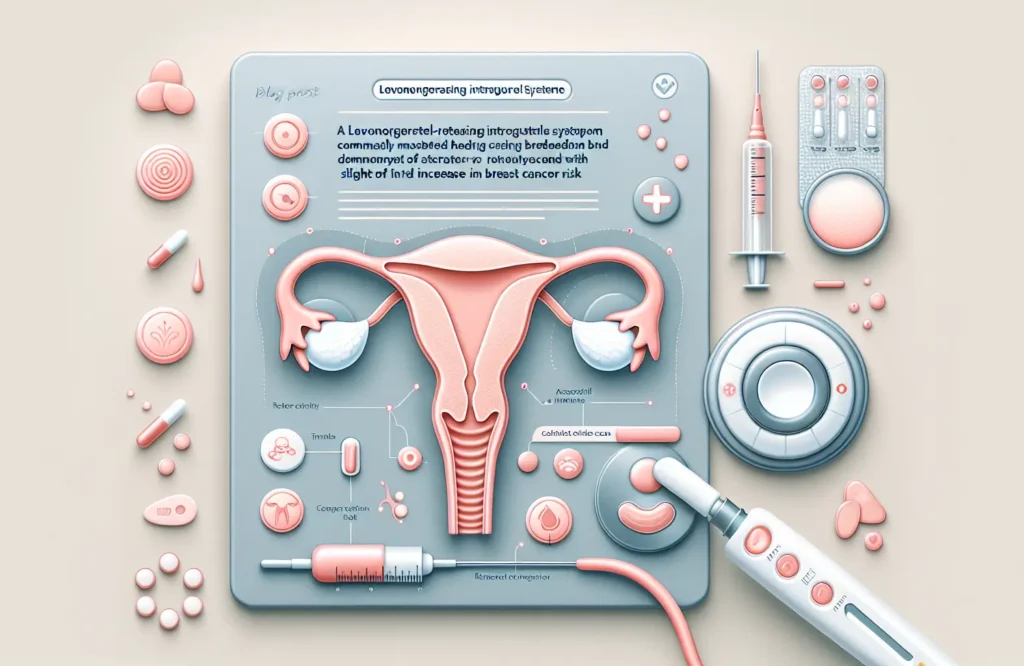
Levonorgestrel-releasing intrauterine systems (LNG-IUS) have become a popular choice for contraception and management of heavy menstrual bleeding due to their efficacy and localized hormone delivery mechanism. Unlike systemic hormone therapies, LNG-IUS devices release progestin directly into the uterine cavity, minimizing systemic hormone levels. However, recent epidemiological studies have raised concerns about a possible association between LNG-IUS use and breast cancer risk, an issue of significant clinical importance given the widespread use of this contraceptive method.
Multiple cohort and case-control studies have examined this potential link, revealing a small but statistically notable increase in breast cancer incidence among current and recent LNG-IUS users compared to non-users. These findings come from diverse populations and have been adjusted for common confounding factors such as age, family history of breast cancer, and the concurrent use of other hormone therapies. Despite this, the absolute risk increase remains low, indicating that while the relative risk might be elevated, the actual number of breast cancer cases attributable directly to LNG-IUS use in any given population is minimal. These nuanced findings highlight the complexity of assessing breast cancer risk in patients using localized hormone therapies and underscore the importance of comprehensive clinical evaluation when advising patients about contraceptive options.
The biological mechanism behind a potential increased breast cancer risk with LNG-IUS use is not fully understood. Levonorgestrel acts primarily within the uterus, but some systemic absorption occurs, potentially influencing breast tissue. Progestins have been shown to impact breast cell proliferation, and their role in breast cancer development remains a topic of ongoing research. Understanding the balance between local effects within the uterus and systemic hormonal exposure is critical to assessing risk. Further studies exploring hormone receptor status in breast tumors of LNG-IUS users and examining dose-response relationships are necessary to elucidate causality and mechanism.
Given the current evidence, clinicians should weigh the benefits of LNG-IUS use against the possible small increase in breast cancer risk, particularly in patients with additional risk factors such as family history or previous breast lesions. Counseling patients about risk should include discussion of this emerging data while emphasizing that LNG-IUS remains a highly effective and generally safe contraceptive method. Regular breast cancer screening and risk assessment should continue according to existing guidelines. Personalized decision-making remains paramount, and ongoing research may further clarify LNG-IUS safety profiles to guide future clinical practice.
Read The Original Publication Here