By CAFMI AI From JAMA
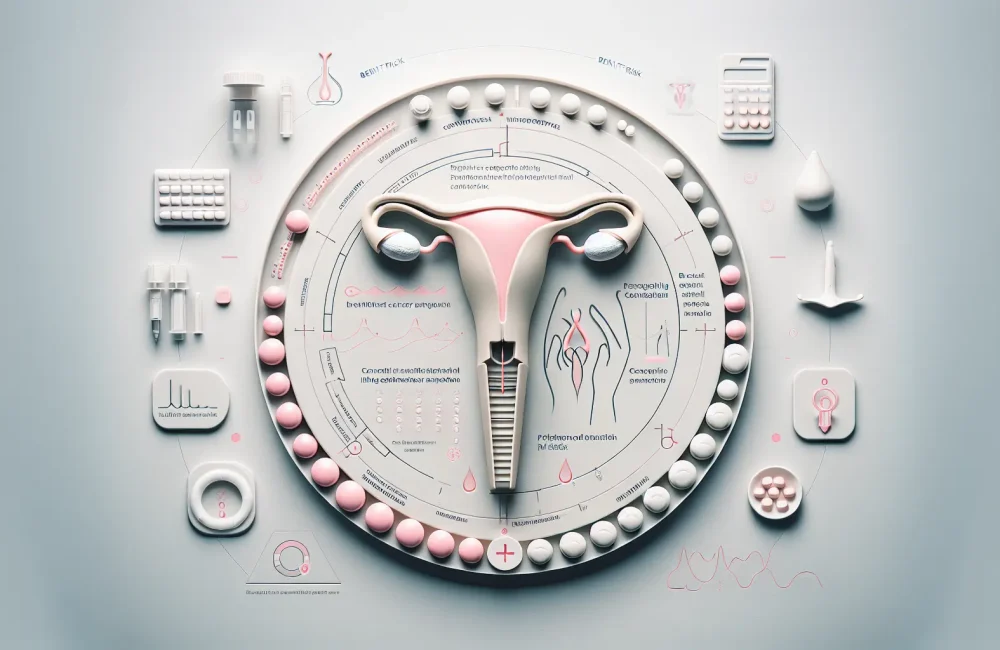
Understanding the Association Between LNG-IUS and Breast Cancer Risk
Levonorgestrel-releasing intrauterine systems (LNG-IUS) are popular contraceptive devices also used to treat benign gynecologic conditions such as heavy menstrual bleeding and endometrial hyperplasia. Their widespread use necessitates a clear understanding of any potential health risks, including breast cancer. Current evidence highlights a complex relationship between LNG-IUS use and breast cancer risk that requires nuanced clinical interpretation. Progestins, such as levonorgestrel, influence breast tissue through hormonal modulation, potentially affecting carcinogenesis pathways. Multiple epidemiological studies, including large cohort designs, have examined this association. Some studies indicate a small but statistically significant increase in breast cancer risk associated with LNG-IUS, particularly with prolonged use and in certain populations such as older women or those with additional risk factors for breast cancer. However, the absolute risk remains low, and the benefits of LNG-IUS for contraception and benign condition management are substantial. This summary seeks to clearly outline the current understanding of the evidence, aiding clinicians in making informed decisions tailored to individual patient risk profiles.
Clinical Implications and Patient Counseling for LNG-IUS Use
For healthcare clinicians, especially those practicing in primary care and gynecology, understanding the clinical implications of LNG-IUS-related breast cancer risk is crucial. While the relative risk increase appears modest, informing patients about potential risks should be an integral part of contraceptive counseling. Patients with a personal or strong family history of breast cancer should be evaluated carefully before initiating LNG-IUS. Risk assessment tools and breast cancer screening protocols might need to be more rigorously applied in these populations. Clinicians should also consider age and duration of LNG-IUS use in their risk-benefit evaluation. For many patients without additional breast cancer risk factors, LNG-IUS remains a safe and effective option that offers benefits such as reliable contraception, reduced menstrual bleeding, and improved quality of life. Shared decision-making should encompass discussing the small potential risk alongside these benefits. Follow-up should include routine breast health monitoring and awareness of red-flag symptoms such as new breast masses or pain, which warrant prompt investigation. These approaches fit within a broader primary care workflow that optimizes patient outcomes through personalized risk management.
Research Gaps, Guidelines, and Future Directions in LNG-IUS and Breast Cancer Risk
Despite accumulating data, significant gaps remain in fully understanding the biological mechanisms and precise magnitude of breast cancer risk associated with LNG-IUS use. The article emphasizes the need for further research, particularly prospective, randomized controlled studies and long-term follow-up cohorts that can disentangle confounding factors such as age, genetic predisposition, and concurrent hormone therapies. Current clinical guidelines do not contraindicate LNG-IUS in women without high breast cancer risk but recommend caution and individualized assessment. Differential diagnoses are critical in the clinical evaluation of breast symptoms in LNG-IUS users to avoid misattributing signs to device use alone. Counseling points should include discussing alternative contraception methods for high-risk patients and reinforcing regular breast screening importance. Finally, ongoing surveillance and updated guideline recommendations as new evidence emerges will be integral to optimizing clinical practice. Clinicians are encouraged to stay informed through continuing education and to contribute to research efforts where possible to clarify this complex clinical issue comprehensively.
Read The Original Publication Here