By CAFMI AI From Nature Reviews Neurology
Clinical Guidelines for AHSCT in MS and NMOSD
**Patient Selection and Treatment Rationale:**
Autologous haematopoietic stem cell transplantation (AHSCT) is emerging as a transformative treatment option for patients with multiple sclerosis (MS) and neuromyelitis optica spectrum disorder (NMOSD), especially in aggressive or treatment-refractory cases. The recent consensus recommendations from the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS) and the European Society for Blood and Marrow Transplantation (EBMT) provide a comprehensive guide for clinicians considering AHSCT. These guidelines emphasize rigorous patient selection criteria that prioritize individuals with active, disabling disease who have failed conventional disease-modifying therapies. The rationale behind AHSCT involves the eradication of the pathogenic immune system and subsequent immune system reset to arrest disease progression. This intervention is particularly considered in relapsing-remitting MS patients with high inflammatory activity but can also be applied cautiously in progressive MS forms where inflammation persists. In NMOSD, the recommendations are more conservative due to limited data but acknowledge potential benefits in refractory cases. The integration of these guidelines into clinical practice promotes standardized care, ensuring optimal therapeutic effects while minimizing complications.
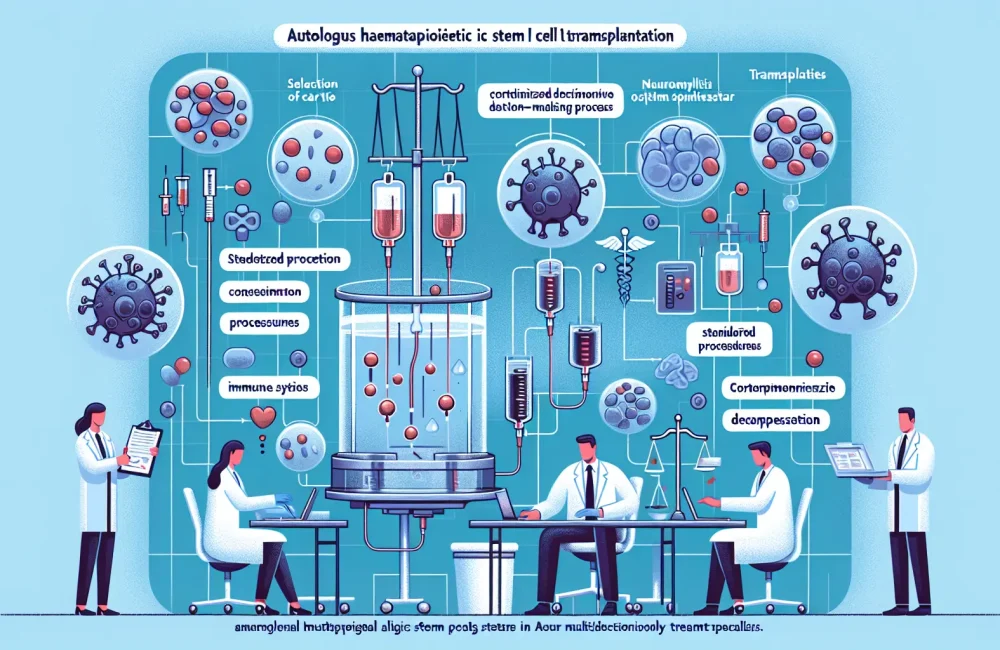
**Procedural Standards and Multidisciplinary Care:**
The guidelines detail standardized procedures for the AHSCT process, highlighting the importance of coordinated multidisciplinary care involving neurologists, hematologists, and transplant specialists. Pre-transplant assessments include thorough evaluation of disease activity, organ function, and infection risks to optimize safety. Mobilization and conditioning regimens are tailored to balance efficacy and toxicity, commonly involving chemotherapy protocols to eradicate autoreactive immune cells while preserving stem cell viability. Post-transplant monitoring focuses on early detection of complications such as infections or secondary autoimmune phenomena and evaluation of neurological outcomes. The document stresses the necessity of experienced centers and specialized teams to conduct AHSCT, underscoring procedural expertise as a critical determinant of patient outcomes. The clinical pathways outlined ensure that patients receive comprehensive care from selection through rehabilitation, encapsulating counseling on risks, benefits, and realistic expectations.
Efficacy and Safety Evidence in Clinical Practice
Recent clinical studies and registry data reviewed in the recommendations robustly support the efficacy of AHSCT in altering the disease course of MS. High rates of no evidence of disease activity (NEDA) have been reported in carefully selected relapsing-remitting MS patients, with sustained neurological improvement and reduced relapse frequency over follow-ups extending beyond five years. The conditioning regimens, ranging from intermediate to high intensity, have demonstrated variable risks but generally acceptable safety profiles, particularly when conducted in experienced centers. Mortality rates have declined over time, reflecting improved protocols and patient selection. The data surrounding AHSCT for NMOSD remain preliminary; however, available case series indicate potential for disease stabilization in refractory patients, warranting further research.
These findings have significant clinical implications. AHSCT offers a potential for durable remission and possibly altering the long-term disability trajectory in MS, an advancement beyond symptomatic or modestly disease-modifying drugs. However, implementing AHSCT requires careful risk-benefit consideration, patient counseling, and post-procedural surveillance. Adverse events such as infection, cytopenias, and secondary autoimmune conditions necessitate vigilance. The recommendations advocate for ongoing data collection and research to refine patient stratification, conditioning regimens, and supportive care measures, aiming to broaden applicability safely and effectively in routine practice.
**Research Gaps and Future Directions:**
While AHSCT is increasingly recognized for its therapeutic potential, the article highlights existing knowledge gaps that underscore the need for continued research. The optimal timing for transplantation, particularly in relation to disease stage and prior treatments, remains to be definitively established. Comparative effectiveness studies versus newer high-efficacy disease-modifying therapies are needed to guide clinical decisions. In NMOSD, more extensive controlled trials are critical to define efficacy and safety profiles.
Future investigations should also explore personalized conditioning approaches that minimize toxicity while maximizing immune reset. Enhanced biomarkers to predict response and monitor outcomes could transform patient selection and follow-up strategies. Furthermore, the consensus encourages integrating AHSCT protocols into multidisciplinary care frameworks within real-world practice and health systems, emphasizing training, infrastructure development, and patient-centered counseling. This forward-looking perspective aims to consolidate the role of AHSCT as a standard care option for carefully selected patients with MS and NMOSD, ultimately improving long-term neurological health and quality of life.
Integrating AHSCT into Routine Neurological Care
To translate the promising outcomes of AHSCT into widespread clinical benefit, the article underscores the importance of infrastructure development and healthcare system readiness. Establishing accredited transplant centers with multidisciplinary expertise is essential to safely deliver AHSCT. Education and training for neurologists, hematologists, and allied health professionals should focus on patient selection, transplant procedures, management of complications, and long-term follow-up.
Patient engagement and counseling stand as pillars to informed decision-making, addressing expectations, potential risks, and benefits. Furthermore, the incorporation of patient-reported outcomes into registries and clinical practice will help personalize treatment approaches and optimize quality of life metrics.
This comprehensive integration calls for collaboration between scientific societies, regulatory bodies, and healthcare providers to create robust guidelines, reimbursement frameworks, and research networks. By building this ecosystem, AHSCT can evolve from a specialized intervention to an accessible, evidence-based treatment modality within the standard neurological care armamentarium for MS and NMOSD.
Read The Original Publication Here