By CAFMI AI From JAMA
Mifepristone Beyond Abortion: Diverse Clinical Roles
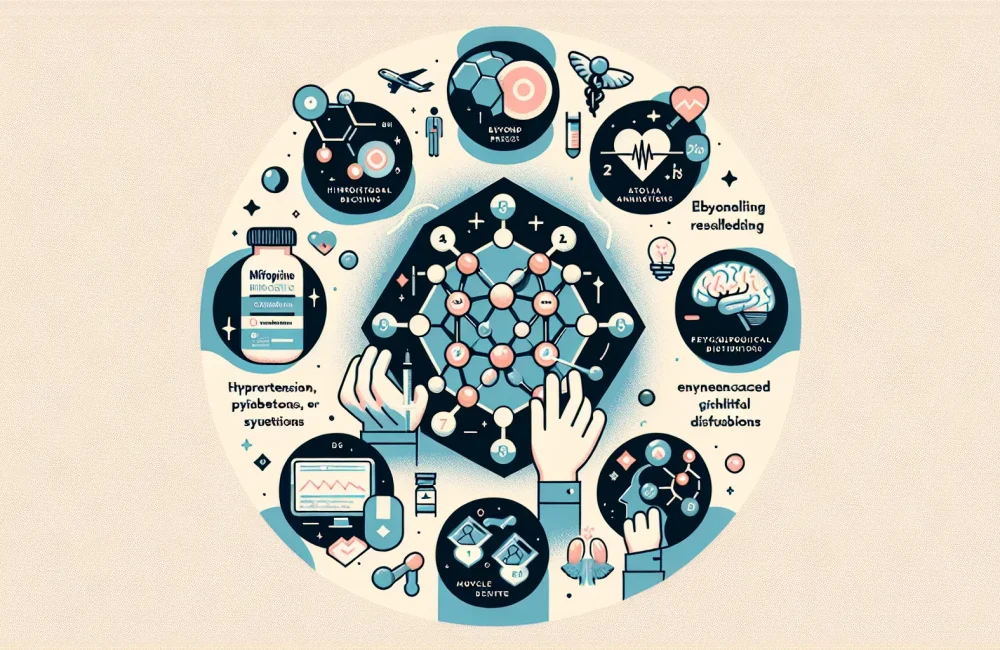
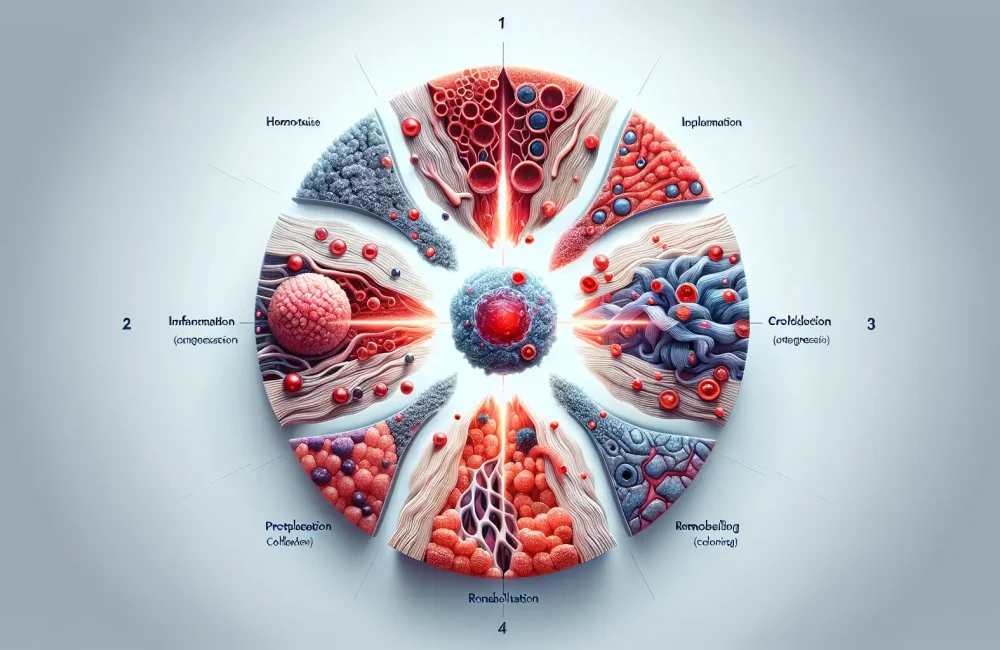
Mifepristone is widely recognized for its use in medical abortion, but its clinical applications extend significantly further, especially relevant to clinicians managing complex conditions in the United States. As a glucocorticoid receptor antagonist, mifepristone offers therapeutic benefits in diseases where cortisol dysregulation is a key factor. One prominent example is Cushing’s syndrome, a disorder caused by chronic exposure to excess cortisol. In this condition, mifepristone blocks cortisol’s effects, helping to alleviate symptoms such as hypertension, diabetes, muscle weakness, and psychological disturbances. This improvement not only enhances patients’ quality of life but may also reduce the burden on healthcare systems by limiting disease complications. The drug’s ability to antagonize glucocorticoid receptors sets it apart from other treatments that solely focus on reducing cortisol production. Thus, mifepristone provides a unique mechanism of action that can be crucial when conventional therapies are ineffective or contraindicated.
Emerging Oncology and Psychiatric Applications of Mifepristone
Recent research highlights mifepristone’s potential roles in oncology and psychiatry, areas where its antiglucocorticoid effects could offer meaningful clinical benefits. In cancer therapy, mifepristone may serve as an adjunct by modulating hormone pathways implicated in tumor growth and progression. This is particularly relevant for cancers influenced by steroid hormones, such as certain breast and prostate cancers. By interfering with glucocorticoid signaling, mifepristone might inhibit tumor proliferation or sensitize cancer cells to other treatments, although more clinical trials are required to establish definitive protocols and efficacy measures. In psychiatry, mifepristone’s role is being explored in mood disorders, especially psychotic depression, where elevated cortisol levels are thought to contribute to symptom severity. Its use could represent a novel therapeutic approach targeting the underlying neuroendocrine dysfunction, offering hope in cases resistant to standard antidepressants or antipsychotics. Given the complexity of these conditions, understanding the nuances of dosing, timing, and patient selection is imperative for clinicians considering mifepristone as part of an integrated treatment plan.
Clinical Implications and Future Directions for Healthcare Providers
For U.S.-based healthcare professionals, recognizing mifepristone’s expanding indications can influence patient management strategies across multiple specialties. The drug’s capacity to target glucocorticoid receptor pathways invites consideration not only in endocrinology but also in oncology, psychiatry, and potentially other fields where cortisol excess or resistance is implicated. Clinicians should stay informed about ongoing clinical trials that are clarifying optimal dosing regimens, safety profiles, and long-term outcomes associated with these newer applications of mifepristone. In practice, careful assessment of patient history, comorbid conditions, and current medications is essential to mitigate risks such as adrenal insufficiency or drug interactions. Counseling patients on realistic expectations, possible side effects, and monitoring requirements is equally important to maximize therapeutic success. Furthermore, primary care workflows may evolve to incorporate screening for conditions amenable to mifepristone treatment, enabling earlier intervention. In summary, mifepristone should be viewed as a versatile pharmaceutical tool with growing potential to improve outcomes in a variety of challenging clinical scenarios beyond its traditional use in abortion care.
Read The Original Publication Here