By CAFMI AI From Frontiers in Medicine (Open Access)
Distinct Sleep Patterns and Their Link to Intrinsic Capacity
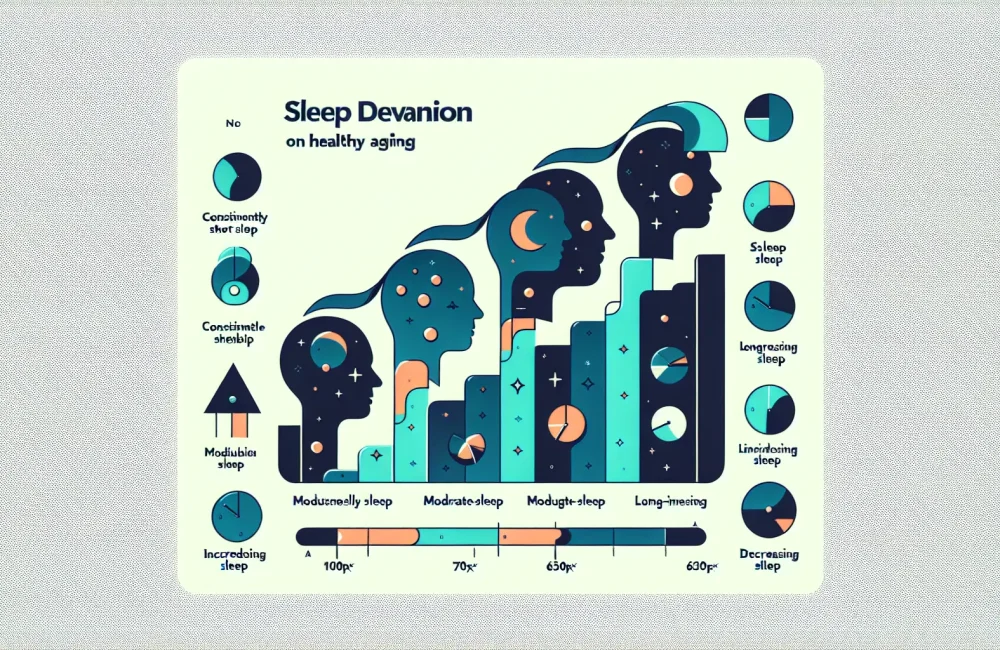
This longitudinal analysis from the China Health and Retirement Longitudinal Study (CHARLS) investigated how varying sleep duration trajectories relate to intrinsic capacity (IC) in middle-aged and older adults. Intrinsic capacity, a comprehensive measure of functional abilities—including locomotion, cognition, vitality, sensory, and psychological domains—is pivotal in understanding healthy aging. The study identified four distinct groups based on sleep duration patterns over multiple waves: consistently short sleep, moderate-stable sleep, long-increasing sleep, and long-decreasing sleep durations. These groupings were derived through rigorous group-based trajectory modeling, allowing refined characterization of how sleep habits evolve over time and their subsequent effects on IC. Importantly, the moderate-stable sleep trajectory served as a reference group due to its association with better functional status in aging adults. This segmentation provides clinicians a nuanced understanding of sleep’s role beyond simple duration snapshots, framing it as a dynamic behavioral and physiological parameter influencing aging outcomes.
Clinical Findings: Sleep Duration’s Effect on Functional Domains
The study’s core finding is that participants with consistently short sleep duration exhibited significantly lower intrinsic capacity scores compared to those in the moderate-stable sleep group, even after controlling for confounding variables such as age, sex, socioeconomic status, and comorbidities. This reduction in IC was broad, affecting multiple domains but was particularly pronounced in areas of vitality and cognitive capacity. Additionally, individuals with long-increasing sleep duration trajectories showed similar declines in total intrinsic capacity, with notable impact on cognition and energy levels. These findings underscore the fact that both abnormally short and increasing long sleep durations over time might signal or contribute to declining functional abilities in aging adults. From a clinical perspective, these patterns alert healthcare providers to the potential underlying physiological or pathological changes reflected in sleep behaviors, emphasizing the need for close monitoring and early interventions.
Implications for Healthcare Practice and Aging Interventions
The implications of this study for clinicians, especially those in primary care and geriatric practice in the USA, highlight the importance of assessing sleep patterns as part of routine evaluations of older adults. Sleep duration is validated as a modifiable risk factor influencing intrinsic capacity and thereby overall functional aging. Intervention strategies should focus on promoting stable, moderate sleep durations to preserve cognitive function, vitality, and general physical performance. This aligns with current healthy aging frameworks that integrate lifestyle and behavioral modifications to mitigate decline. Clinicians should incorporate sleep hygiene counseling, screening for sleep disorders, and possibly refer patients for tailored sleep therapy when deviations from moderate-stable patterns occur. Furthermore, regular follow-up on sleep habits can serve as a prognostic tool to evaluate the trajectory of aging and functional decline. Given the associations observed, understanding and addressing sleep duration may also help discern differential diagnoses and flag red flags related to neurological or psychiatric disorders in the aging population. Collectively, the study advocates for embedding sleep assessment into comprehensive geriatric workflows to foster healthier aging trajectories and enhance quality of life.
Read The Original Publication Here