By CAFMI AI From npj Parkinson’s Disease (Open Access)
Digestive Diseases as Early Indicators of Parkinson’s Disease
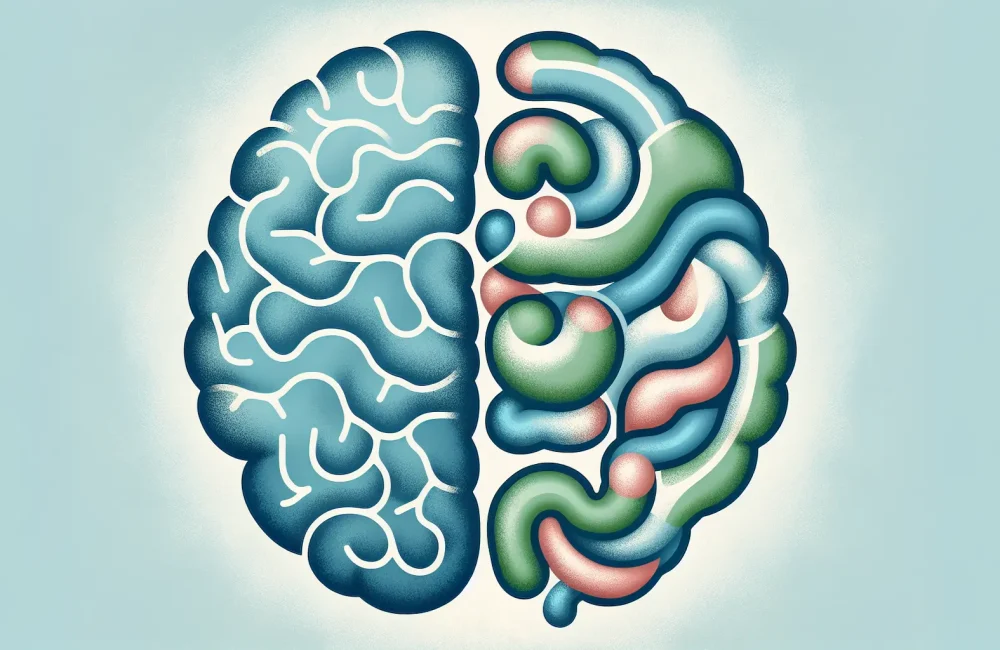
Parkinson’s disease (PD) is a complex neurodegenerative disorder traditionally characterized by its motor symptoms but increasingly recognized for its prodromal, non-motor features, particularly digestive and gastrointestinal dysfunctions. This article highlights groundbreaking evidence linking digestive diseases—such as gastroesophageal reflux disease (GERD), irritable bowel syndrome (IBS), and inflammatory bowel disease (IBD)—to an increased risk of developing PD. These digestive disorders are often accompanied by chronic inflammation and alterations in gut microbiota, factors believed to contribute to the neuropathological changes seen in PD through the gut-brain axis. By analyzing a large cohort with robust statistical models that adjust for confounders, researchers demonstrated that individuals with a history of such digestive diseases show a significantly elevated risk of PD onset. This finding reinforces the clinical observation that gastrointestinal symptoms frequently precede the classic motor manifestations, often by years. For clinicians, especially those working within primary care and neurology in the USA, recognizing and monitoring digestive disease symptoms may provide a crucial opportunity for earlier identification of patients at risk, potentially allowing for earlier diagnostic evaluation, surveillance, and targeted counseling.
Influence of Lifestyle Factors on Parkinson’s Disease Risk
The study further explored crucial lifestyle factors—diet, physical activity, smoking, and alcohol consumption—and their modifying effects on PD risk, particularly in the context of prior digestive disease exposure. Regular physical exercise and adherence to a healthy diet emerged as significant protective factors against PD. These lifestyle habits likely influence the disease risk by modulating systemic inflammation levels and gut microbiota composition, thereby potentially mitigating neuroinflammatory processes implicated in PD pathogenesis. Contrasting with these protective elements, smoking exhibited a complex association; while some epidemiological studies suggest a paradoxical inverse relationship with PD, this study cautions about potential confounding variables that might influence such outcomes. Alcohol consumption’s role was less clearly defined but is considered within the broader lifestyle context. For healthcare professionals, promoting physical activity and nutritional counseling becomes a vital part of preventive care aimed at reducing PD risk, particularly in patients with digestive disease histories.
Clinical Implications and Future Directions
The findings emphasize the importance of integrating digestive health assessment and lifestyle evaluation into routine clinical practice for Parkinson’s disease risk stratification. Early recognition of gastrointestinal symptoms and digestive disorders should prompt neurologists and primary care providers to consider PD risk and implement surveillance or preventive strategies. Moreover, fostering healthy lifestyle behaviors such as exercise and proper nutrition could serve as adjunctive interventions to delay or reduce PD onset, especially for those with a history of digestive diseases. Future research is encouraged to further elucidate the mechanistic links between the gut-brain axis and PD pathogenesis, optimize lifestyle intervention protocols, and establish standardized screening guidelines to enhance early diagnosis and improve patient outcomes.
Read The Original Publication Here