By CAFMI AI From Frontiers in Medicine (Open Access)
Systemic Inflammation and COPD: Understanding the Mediator Role of SIRI
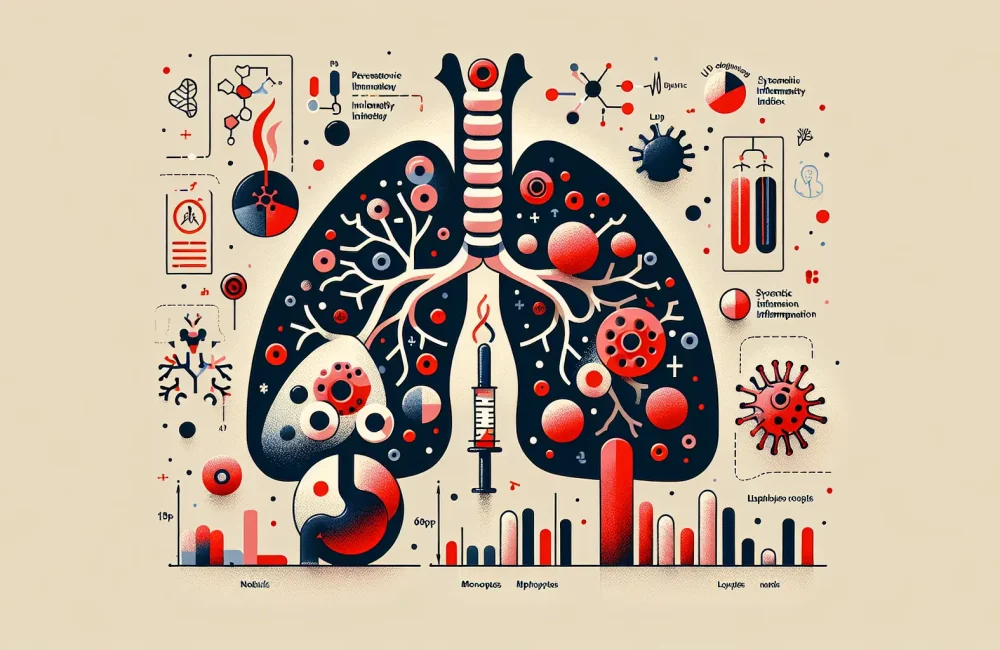
Chronic obstructive pulmonary disease (COPD) remains a leading cause of morbidity and mortality globally, with persistent airflow limitation and chronic pulmonary inflammation as defining features. Clinicians recognize that inflammation plays a central role in the disease’s pathogenesis, yet identifying precise biomarkers to facilitate early diagnosis and monitor disease progression remains a clinical priority. Recent research has focused on the systemic inflammatory response and its contribution to COPD severity, prompting investigation into composite biomarkers that reflect systemic inflammation beyond localized lung inflammation. One such biomarker, the Systemic Inflammatory Response Index (SIRI), combines neutrophil, monocyte, and lymphocyte counts into a single inflammatory metric. This amalgamation potentially offers a more holistic view of systemic inflammation relevant to COPD progression.
The featured study investigates SIRI as a mediator between Lymphocyte Count 9 (LC9), a novel lymphocyte subtype implicated in inflammatory regulation, and COPD development. LC9, as part of the broader immune response, is believed to influence inflammatory processes in COPD, but the pathway of this influence was unclear before this study. By evaluating the mediation effect of SIRI, the study aimed to unravel this immunological relationship, offering clinicians a clearer understanding of the inflammatory pathways active in COPD through systemic indices like SIRI. This approach represents an advancement over traditional single-cell count analyses, emphasizing integrated immune response indices for clinical insights.
Key Findings: Linking LC9, SIRI, and COPD Severity
The methodology involved recruiting a cohort of patients diagnosed with COPD alongside control subjects without the disease to ensure comparative analysis. Blood specimens were collected from all participants to quantify LC9 levels and calculate SIRI values. The statistical approach centered on mediation analysis, a technique that assesses if the relationship between an independent variable (LC9) and an outcome (COPD severity) occurs partially or wholly through a mediator variable (SIRI).
Results demonstrated that patients with COPD exhibited significantly altered LC9 levels compared to healthy controls, indicating dysregulated lymphocyte subpopulations associated with the disease. More notably, SIRI values were markedly elevated in COPD patients, corroborating systemic inflammation’s critical role in disease pathology. Mediation analysis confirmed that SIRI partially mediates the relationship between LC9 and COPD. This means that part of LC9’s effect on COPD severity is transmitted through systemic inflammation as measured by SIRI, highlighting SIRI not only as a biomarker but also as an active participant in disease progression.
Clinically, these findings suggest that monitoring SIRI could provide valuable information about the inflammatory status and potential disease trajectory in COPD patients. The implication is significant — it supports integrating systemic inflammatory markers into routine assessments, which could lead to earlier identification of disease exacerbation risks and better-informed management strategies.
Clinical Implications and Future Directions for COPD Management
Understanding SIRI’s mediating role in the LC9-COPD relationship informs several key clinical considerations. First, systemic inflammation is reaffirmed as a cornerstone of COPD pathogenesis, and composite inflammatory indices like SIRI capture this complex immunological environment more effectively than isolated biomarkers. This knowledge encourages clinicians to consider multi-parameter inflammatory markers for patient evaluation rather than relying solely on conventional markers such as C-reactive protein or isolated leukocyte counts.
Second, the identification of LC9 and SIRI as interconnected components in COPD pathology opens avenues for targeted therapeutic interventions. Anti-inflammatory strategies aiming to modulate systemic inflammation might be optimized by focusing on pathways reflected through SIRI measurements. Personalized medicine approaches can be designed to attenuate inflammation in patients exhibiting high SIRI and altered LC9 profiles, potentially slowing disease progression and reducing exacerbation frequency.
Finally, the study highlights the need for further longitudinal research to validate the utility of SIRI and LC9 in clinical practice. Evaluation of these markers in larger, diverse patient populations and integration with other clinical parameters could enhance risk stratification and tailor treatment protocols. For primary care and pulmonary specialists, incorporating systematic inflammatory assessments might transform COPD management workflows, enabling better counseling on disease progression, medication adherence, and follow-up intervals tailored to inflammation status. In summary, recognizing SIRI as a mediator between LC9 and COPD extends our understanding of disease mechanisms and offers a promising path toward improved patient outcomes through refined diagnostic and treatment strategies.
Read The Original Publication Here