By CAFMI AI From JAMA
Supine Hypertension: An Overlooked Cardiovascular Risk Factor
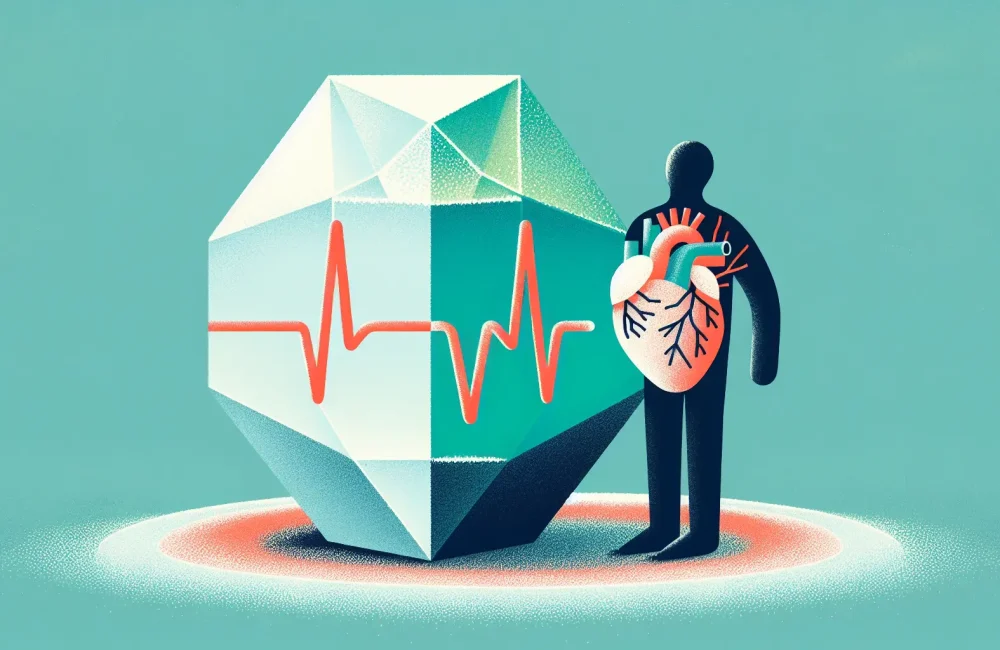
Supine hypertension, defined as elevated blood pressure when lying down, represents an important but often overlooked cardiovascular risk factor. Traditionally, blood pressure assessment focuses on seated measurements, which may fail to capture critical risks associated with blood pressure changes in other positions. This study aimed to evaluate whether supine hypertension independently contributes to cardiovascular events and mortality, regardless of seated blood pressure levels. The longitudinal study involved adult participants who had their blood pressure monitored in both seated and supine positions over an extended follow-up period. Researchers observed the incidence of major cardiovascular events, including heart attacks, strokes, and cardiovascular mortality. Their findings revealed that individuals exhibiting supine hypertension were at significantly increased risk of these adverse cardiovascular outcomes, even when seated blood pressure was within a normal range. This discovery challenges current clinical practices that rely predominantly on seated blood pressure measurements for risk assessment and management, potentially missing a subset of patients at heightened risk due to elevated supine pressures.
Clinical Implications and Recommendations for Blood Pressure Monitoring
The clinical implications of recognizing supine hypertension as an independent risk factor are substantial for healthcare providers, especially those working in primary care and cardiology settings. First, routine blood pressure measurement protocols may need expansion to include supine readings, particularly in patients with risk factors for cardiovascular diseases but normal seated blood pressure. Integrating supine blood pressure assessments could improve risk stratification, allowing clinicians to identify high-risk individuals who might otherwise appear normotensive under current measurement practices. Additionally, these findings underscore the necessity for updated clinical guidelines to incorporate positional blood pressure measurements. This includes training healthcare professionals on the significance of supine hypertension and its evaluation techniques. Early detection of supine hypertension could lead to more tailored treatment strategies, potentially involving lifestyle modifications or pharmacologic therapy aimed at controlling nocturnal or supine blood pressure elevations. Moreover, clinicians should be vigilant for symptoms or signs suggestive of labile or positional hypertension, which may warrant comprehensive evaluation.
Broader Context, Limitations, and Future Directions
While this study provides important insights, several considerations should guide clinical application. The cohort primarily consisted of adults undergoing longitudinal monitoring, but factors such as age, comorbid conditions, and medication use may influence blood pressure dynamics and cardiovascular risk differently across populations. Moreover, the specific thresholds defining supine hypertension require further validation to standardize diagnosis and treatment. Understanding the mechanisms driving supine hypertension, such as autonomic dysfunction or volume status changes during recumbency, remains an area for future research. Clinicians should also be aware of differential diagnoses, including white coat hypertension or masked hypertension, which can complicate interpretation. From a practical standpoint, incorporating supine blood pressure measurements in clinical workflows demands procedural adjustments and patient counseling to ensure accurate and reproducible readings. Educating patients about positional blood pressure variations and their cardiovascular implications supports better adherence to monitoring and treatment regimens. Ultimately, this study advocates for a paradigm shift in blood pressure monitoring strategies, emphasizing comprehensive positional assessments to enhance cardiovascular risk prediction and patient outcomes.
Read The Original Publication Here