By CAFMI AI From npj Parkinson’s Disease (Open Access)
Invasive Neuromodulation Advances
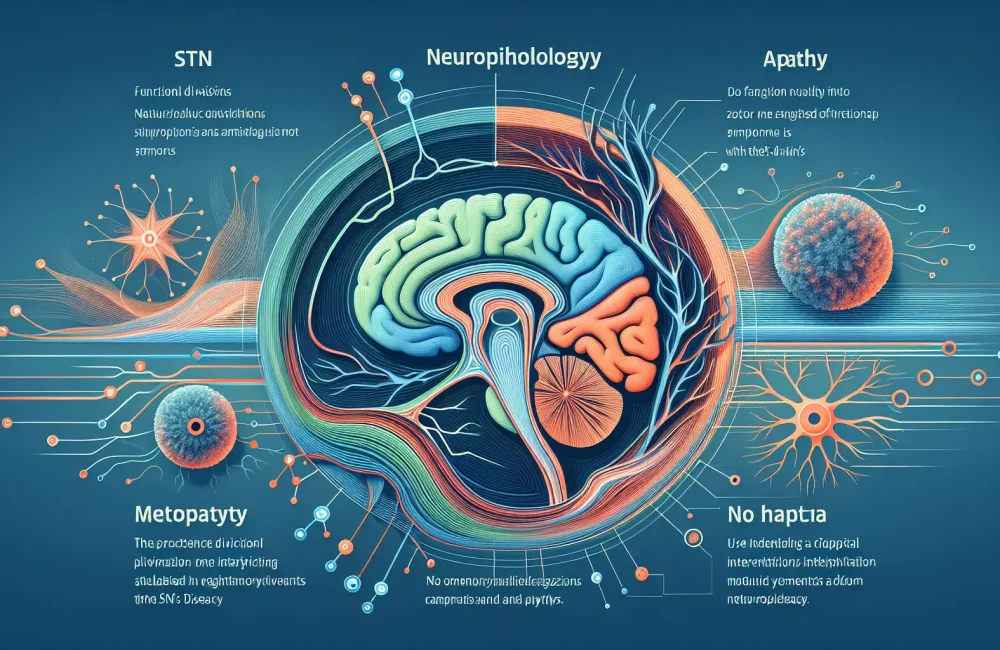
Deep brain stimulation (DBS) remains a cornerstone of invasive neuromodulation for Parkinson’s disease (PD), offering robust improvements in motor symptoms like tremor, rigidity, and bradykinesia. Implantation of electrodes in brain areas such as the subthalamic nucleus and globus pallidus internus helps reduce patients’ medication needs and improve mobility. Recently, technological advances including directional leads and adaptive stimulation systems have enhanced the precision of DBS, allowing real-time adjustment to patient neural activity and further optimizing symptom control. Novel targets, such as the pedunculopontine nucleus, are also being explored to address gait and balance problems that traditional targets do not fully resolve. While DBS predominantly benefits motor symptoms, effects on non-motor symptoms such as mood and cognition are less consistent, signaling areas for future research.
Non-Invasive Neuromodulation Techniques
Non-invasive neuromodulation offers promising alternatives for PD patients who may not qualify for surgery or prefer less invasive options. Techniques like transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) aim to modulate cortical activity to improve both motor and cognitive function. Although clinical trials show mixed results to date, refinement of stimulation parameters — including site, intensity, and timing — continues to improve outcomes. Focused ultrasound has recently gained attention as a non-invasive method capable of targeting deep brain structures without open surgery, potentially expanding therapeutic options for symptom control, especially for those with medication-refractory tremor or rigidity.
Future Directions and Clinical Implications
The future of neuromodulation in PD is moving toward personalized medicine, integrating sophisticated neuroimaging and biomarkers to tailor treatments to individual patients’ pathophysiology. Closed-loop systems that adjust stimulation based on real-time feedback and machine learning algorithms promise greater effectiveness and minimization of side effects. Furthermore, expanding neuromodulation targets to address non-motor symptoms is a critical development, as these symptoms—such as cognitive decline, mood disorders, and autonomic dysfunction—dramatically affect quality of life. For primary care physicians, awareness of emerging neuromodulation innovations is vital, as these therapies may become increasingly relevant for patient referrals, post-treatment management, and discussing therapeutic options with patients. Overall, neuromodulation represents a rapidly evolving therapeutic frontier with significant potential to improve patient outcomes in PD.
Read The Original Publication Here