By CAFMI AI From npj Gut and Liver (Open Access)
Dual Nature of MetALD Explained
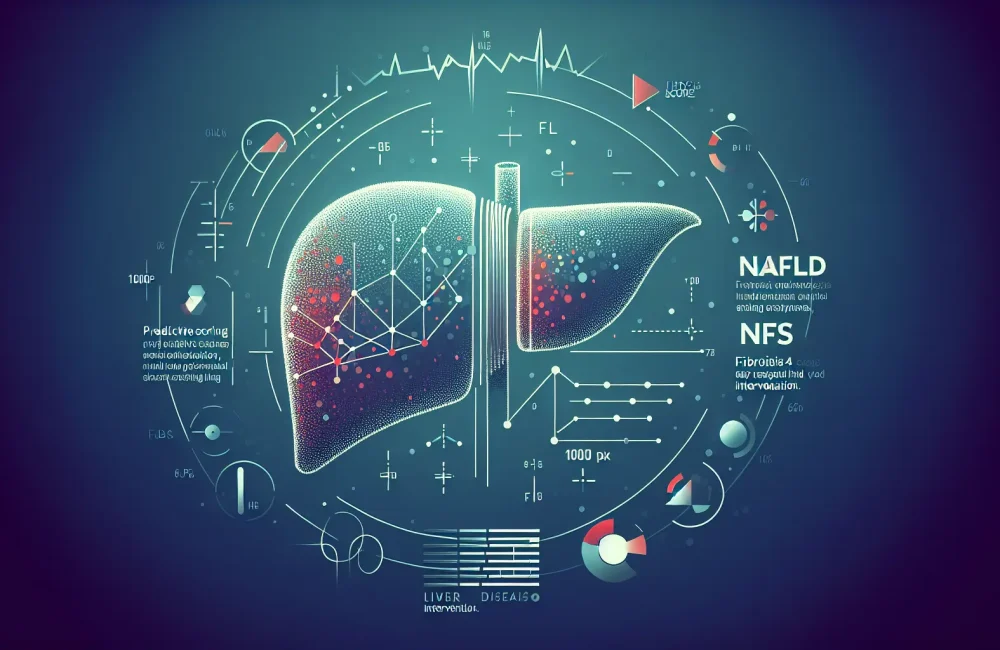
Metabolic and alcohol-associated liver disease, termed MetALD, represents a complex overlap of liver damage caused by both metabolic dysfunction and alcohol use. This dual etiology challenges traditional liver disease classifications that separate conditions into either metabolic or alcohol-related categories, often missing the significant number of patients affected by both. Understanding MetALD is crucial for primary care clinicians since it affects diagnosis, treatment, and patient outcomes. The article highlights that liver injury in MetALD arises from intertwined molecular mechanisms involving inflammation, fibrosis, and disrupted metabolism. Recognizing this interplay guides more accurate diagnosis and patient management, underlining the need for clinicians to consider both metabolic and alcohol-related factors when evaluating liver health.
Clinical Implications and Diagnostic Challenges
Clinically, MetALD manifests with symptoms and signs typical of liver injury but can be more severe due to the combined metabolic and alcohol effects. Patients may present with elevated liver enzymes and fibrosis markers, but typical diagnostic criteria often fail to capture this dual pathology comprehensively. The article stresses the importance of developing refined biomarkers to detect MetALD early and accurately. For primary care providers, this means heightened vigilance and possibly new screening protocols for patients with both metabolic syndrome and a history of alcohol use. Early and precise identification of MetALD can lead to more tailored therapeutic approaches, improving patient prognoses by addressing both metabolic dysfunction and alcohol impact together.
Toward Personalized Management and Future Directions
Management strategies for MetALD must integrate lifestyle interventions addressing metabolic syndrome and alcohol cessation programs, as these patients do not respond well to treatments targeting only one cause. The article advocates for personalized care plans that consider the dual nature of MetALD to prevent disease progression and complications like cirrhosis. Research is pushing toward refining liver disease classifications and developing combined therapeutic pathways that reduce inflammation and fibrosis from both metabolic and alcohol origins. For primary care clinicians, staying informed about this evolving paradigm and participating in multidisciplinary care models may significantly improve patient outcomes. The article suggests that future clinical guidelines will likely incorporate MetALD more explicitly, assisting primary care physicians in risk stratification and management.
Read The Original Publication Here