By CAFMI AI From Nature Reviews Neurology
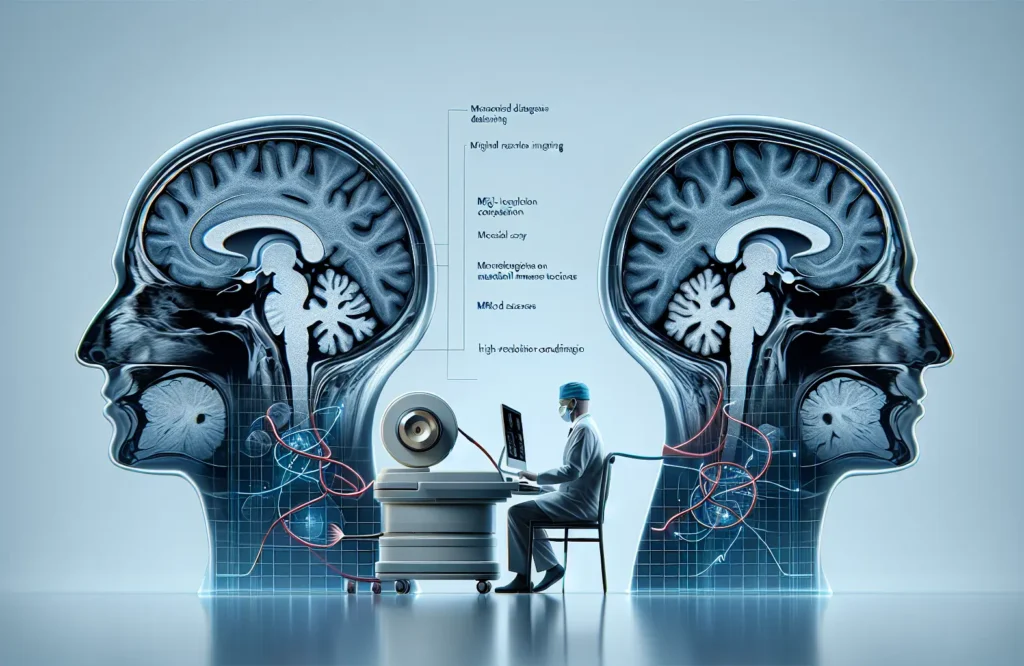
The 2024 revision of the McDonald criteria for multiple sclerosis (MS) represents a pivotal update designed to improve the accuracy and timeliness of MS diagnosis, a crucial aspect for clinicians managing this complex neurological disorder. Central to these revisions is the incorporation of advanced magnetic resonance imaging (MRI) techniques that significantly enhance the detection of MS lesions. The guidelines now emphasize the use of high-resolution MRI with standardized sequences tailored to identify lesions more reliably in characteristic central nervous system (CNS) regions. This refinement in MRI protocols is essential for demonstrating dissemination in space (DIS), a key diagnostic requirement indicating lesion presence in multiple CNS areas commonly affected by MS. Moreover, dissemination in time (DIT) criteria have been updated to allow diagnosis based on either simultaneous presence of both enhancing and non-enhancing lesions or through identification of new lesion development on subsequent scans. This nuanced approach allows for earlier and more definitive diagnosis than previous criteria. From a practical standpoint, these imaging advancements equip neurologists and radiologists with precise tools to differentiate MS lesions from other CNS abnormalities, facilitating improved diagnostic confidence. In clinical workflows, integrating these updated MRI standards will likely require coordination between imaging specialists and neuroimmunologists to ensure that scan protocols meet recommended resolutions and sequences. Overall, these imaging-centric updates address prior diagnostic challenges by balancing sensitivity and specificity, aiming to reduce both underdiagnosis and misdiagnosis of MS, which is paramount for early intervention and long-term patient management.
Beyond imaging, the 2024 McDonald criteria revision highlights the critical role of biomarkers and comprehensive clinical assessment in confirming MS diagnosis, particularly when imaging alone is inconclusive. One prominent biomarker now included is cerebrospinal fluid (CSF) analysis for oligoclonal bands, which provides supportive evidence of intrathecal IgG synthesis indicative of MS-related inflammation. Incorporating CSF oligoclonal band testing is especially valuable when MRI findings do not fully satisfy dissemination requirements but clinical suspicion remains high. Additionally, serum neurofilament light chain (sNfL) levels have emerged as a promising biomarker reflecting neuroaxonal damage and disease activity. Although sNfL measurement is not yet universally standard, its integration into diagnostic frameworks offers potential for prognostication and monitoring. Clinicians should consider these laboratory markers alongside clinical presentations—such as relapsing or primary progressive symptoms—to guide diagnostic decision-making. The revised criteria also address differential diagnosis more robustly, urging careful exclusion of MS mimics like neuromyelitis optica spectrum disorders and other inflammatory or infectious diseases. This multifaceted approach, combining clinical signs, radiological findings, and biomarkers, enables earlier and more accurate MS diagnoses, ultimately guiding timely therapeutic interventions. For primary care providers and specialists alike, understanding and applying these integrated criteria can enhance patient counseling regarding diagnosis, prognosis, and treatment planning.
The 2024 McDonald criteria not only refine diagnosis but also have meaningful implications for treatment initiation and long-term management of MS. Accurate and earlier diagnosis facilitated by the updated criteria allows clinicians to implement disease-modifying therapies (DMTs) sooner, which is critical for reducing relapse rates and slowing disability progression. The criteria’s emphasis on integrating imaging and biomarkers supports tailored treatment strategies based on disease activity and prognosis. Furthermore, clear diagnostic pathways help identify patients with primary progressive MS, who may benefit from differing therapeutic approaches. The criteria also encourage ongoing monitoring using updated MRI and biomarker assessments to evaluate treatment response and disease progression over time. For patients, these advancements mean quicker access to appropriate therapies and more informed discussions about disease course and lifestyle adjustments. Clinicians are advised to integrate the revised criteria into multidisciplinary care models to optimize outcomes, highlighting the evolving landscape in MS diagnosis and management that prioritizes precision medicine and personalized care.
Read The Original Publication Here